

Chinese General Practice ›› 2025, Vol. 28 ›› Issue (12): 1459-1464.DOI: 10.12114/j.issn.1007-9572.2024.0118
Special Issue: 老年人群健康最新文章合辑; 老年问题最新文章合辑
• Original Research • Previous Articles Next Articles
Received:2024-04-25
Revised:2024-06-19
Published:2025-04-20
Online:2025-02-06
Contact:
GUO Shubin
通讯作者:
郭树彬
作者简介:作者贡献:
李秋敬负责研究设计、数据收集、统计分析、论文撰写;商娜进行数据收集与整理、论文修订;高倩、杨黎进行数据收集、统计分析指导;郭树彬负责论文审校、质量控制,对文章整体负责。所有作者确认了论文的最终稿。
基金资助:CLC Number:
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.chinagp.net/EN/10.12114/j.issn.1007-9572.2024.0118
| 项目 | 生存组(n=250) | 死亡组(n=85) | 检验统计量值 | P值 |
|---|---|---|---|---|
| 年龄[M(P25,P75),岁] | 76(69,84) | 82(75,88) | 3.745 | <0.001 |
| 性别[例(%)] | 0.010a | 0.979 | ||
| 男 | 121(48.4) | 41(48.2) | ||
| 女 | 129(51.6) | 44(51.8) | ||
| BMI(kg/m2) | 23.4±3.6 | 22.0±3.8 | -3.179b | 0.002 |
| 基础疾病[例(%)] | ||||
| 高血压 | 123(49.2) | 52(61.2) | 3.647a | 0.056 |
| 冠状动脉粥样硬化性心脏病 | 76(30.4) | 25(29.4) | 0.029a | 0.864 |
| 2型糖尿病 | 94(37.6) | 29(34.1) | 0.331a | 0.565 |
| 恶性肿瘤 | 40(16.0) | 21(24.7) | 3.228a | 0.072 |
| 慢性肾脏病 | 33(13.2) | 17(20.0) | 2.310a | 0.129 |
| 慢性肺部疾病 | 21(8.4) | 8(9.4) | 0.082a | 0.774 |
| 慢性肝脏疾病 | 11(4.4) | 4(4.7) | 0.014a | 0.906 |
| 实验室检查指标[M(P25,P75)] | ||||
| 白细胞计数(×109/L) | 10.88(7.11,14.30) | 10.37(7.39,16.63) | 0.943 | 0.346 |
| 中性粒细胞计数(×109/L) | 8.76(5.06,12.81) | 9.19(6.25,14.77) | 1.169 | 0.243 |
| 血红蛋白(g/L) | 121(103,138) | 116(84,137) | -1.959 | 0.050 |
| 血小板计数(×109/L) | 189(137,240) | 181(119,257) | -0.561 | 0.575 |
| 白蛋白(g/L) | 37.3(33.3,41.5) | 33.5(29.5,39.2) | -4.283 | <0.001 |
| 肌酐(μmol/L) | 83.6(63.2,129.6) | 140.3(74.5,244.4) | 3.730 | <0.001 |
| D-二聚体(mg/L) | 2.11(1.21,3.82) | 2.11(1.60,6.52) | 1.757 | 0.079 |
| 降钙素原(ng/mL) | 0.81(0.16,2.22) | 0.81(0.36,7.23) | 2.123 | 0.034 |
| L3 SMI[M(P25,P75),cm2/m2] | 34.82(30.19,41.26) | 30.38(24.78,32.87) | -5.817 | <0.001 |
| NRS2002评分[M(P25,P75),分] | 3(2,4) | 4(4,6) | 6.526 | <0.001 |
| 脓毒性休克[例(%)] | 70(28.0) | 46(54.1) | 19.115a | <0.001 |
| SOFA评分[M(P25,P75),分] | 3(2,5) | 6(4,9) | 6.820 | <0.001 |
| APACHE Ⅱ评分[M(P25,P75),分] | 11(6,15) | 17(11,24) | 6.688 | <0.001 |
| 住院时间[M(P25,P75),d] | 10(6,14) | 8(3,18) | -1.053 | 0.293 |
Table 1 Comparison of clinical characteristics between survival and non-survival group among older patients with intra-abdominal sepsis
| 项目 | 生存组(n=250) | 死亡组(n=85) | 检验统计量值 | P值 |
|---|---|---|---|---|
| 年龄[M(P25,P75),岁] | 76(69,84) | 82(75,88) | 3.745 | <0.001 |
| 性别[例(%)] | 0.010a | 0.979 | ||
| 男 | 121(48.4) | 41(48.2) | ||
| 女 | 129(51.6) | 44(51.8) | ||
| BMI(kg/m2) | 23.4±3.6 | 22.0±3.8 | -3.179b | 0.002 |
| 基础疾病[例(%)] | ||||
| 高血压 | 123(49.2) | 52(61.2) | 3.647a | 0.056 |
| 冠状动脉粥样硬化性心脏病 | 76(30.4) | 25(29.4) | 0.029a | 0.864 |
| 2型糖尿病 | 94(37.6) | 29(34.1) | 0.331a | 0.565 |
| 恶性肿瘤 | 40(16.0) | 21(24.7) | 3.228a | 0.072 |
| 慢性肾脏病 | 33(13.2) | 17(20.0) | 2.310a | 0.129 |
| 慢性肺部疾病 | 21(8.4) | 8(9.4) | 0.082a | 0.774 |
| 慢性肝脏疾病 | 11(4.4) | 4(4.7) | 0.014a | 0.906 |
| 实验室检查指标[M(P25,P75)] | ||||
| 白细胞计数(×109/L) | 10.88(7.11,14.30) | 10.37(7.39,16.63) | 0.943 | 0.346 |
| 中性粒细胞计数(×109/L) | 8.76(5.06,12.81) | 9.19(6.25,14.77) | 1.169 | 0.243 |
| 血红蛋白(g/L) | 121(103,138) | 116(84,137) | -1.959 | 0.050 |
| 血小板计数(×109/L) | 189(137,240) | 181(119,257) | -0.561 | 0.575 |
| 白蛋白(g/L) | 37.3(33.3,41.5) | 33.5(29.5,39.2) | -4.283 | <0.001 |
| 肌酐(μmol/L) | 83.6(63.2,129.6) | 140.3(74.5,244.4) | 3.730 | <0.001 |
| D-二聚体(mg/L) | 2.11(1.21,3.82) | 2.11(1.60,6.52) | 1.757 | 0.079 |
| 降钙素原(ng/mL) | 0.81(0.16,2.22) | 0.81(0.36,7.23) | 2.123 | 0.034 |
| L3 SMI[M(P25,P75),cm2/m2] | 34.82(30.19,41.26) | 30.38(24.78,32.87) | -5.817 | <0.001 |
| NRS2002评分[M(P25,P75),分] | 3(2,4) | 4(4,6) | 6.526 | <0.001 |
| 脓毒性休克[例(%)] | 70(28.0) | 46(54.1) | 19.115a | <0.001 |
| SOFA评分[M(P25,P75),分] | 3(2,5) | 6(4,9) | 6.820 | <0.001 |
| APACHE Ⅱ评分[M(P25,P75),分] | 11(6,15) | 17(11,24) | 6.688 | <0.001 |
| 住院时间[M(P25,P75),d] | 10(6,14) | 8(3,18) | -1.053 | 0.293 |
| 变量 | β | SE | Wald χ2值 | OR值 | 95%CI | P值 |
|---|---|---|---|---|---|---|
| L3 SMI | -0.079 | 0.021 | 13.569 | 0.924 | 0.886~0.964 | <0.001 |
| NRS2002评分 | 0.271 | 0.097 | 7.898 | 1.312 | 1.086~1.585 | 0.005 |
| SOFA评分 | 0.157 | 0.054 | 8.516 | 1.170 | 1.053~1.300 | 0.004 |
| APACHE Ⅱ评分 | 0.051 | 0.024 | 4.305 | 1.052 | 1.003~1.103 | 0.038 |
| 常数项 | -1.129 | 0.875 | 1.663 | 0.323 | 0.197 |
Table 2 Multivariable Logistic regression analysis of risk factors associated with in-hospital mortality among older patients with intra-abdominal sepsis
| 变量 | β | SE | Wald χ2值 | OR值 | 95%CI | P值 |
|---|---|---|---|---|---|---|
| L3 SMI | -0.079 | 0.021 | 13.569 | 0.924 | 0.886~0.964 | <0.001 |
| NRS2002评分 | 0.271 | 0.097 | 7.898 | 1.312 | 1.086~1.585 | 0.005 |
| SOFA评分 | 0.157 | 0.054 | 8.516 | 1.170 | 1.053~1.300 | 0.004 |
| APACHE Ⅱ评分 | 0.051 | 0.024 | 4.305 | 1.052 | 1.003~1.103 | 0.038 |
| 常数项 | -1.129 | 0.875 | 1.663 | 0.323 | 0.197 |
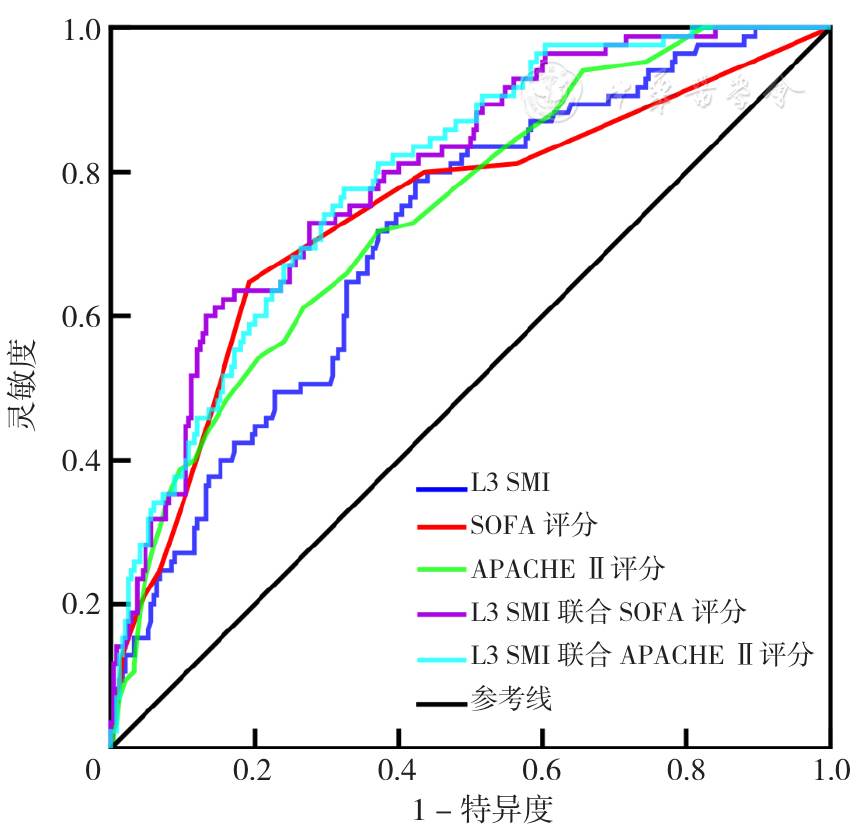
Figure 2 The ROC curves of L3 SMI,SOFA score,APACHE Ⅱ score and combined variables on the risk of in-hospital mortality in older patients with intra-abdominal sepsis
| 变量 | AUC(95%CI) | 最佳截断值 | 约登指数 | 灵敏度 | 特异度 | P值 |
|---|---|---|---|---|---|---|
| L3 SMI | 0.711(0.650~0.772) | 33.30 cm2/m2 | 0.364 | 0.788 | 0.576 | <0.001 |
| SOFA评分 | 0.740(0.675~0.806) | 5.5分 | 0.455 | 0.647 | 0.808 | <0.001 |
| APACHE Ⅱ评分 | 0.742(0.684~0.801) | 12.5分 | 0.346 | 0.718 | 0.628 | <0.001 |
| L3 SMI联合SOFA评分 | 0.795(0.742~0.847) | 0.336 | 0.468 | 0.600 | 0.868 | <0.001 |
| L3 SMI联合APACHE Ⅱ评分 | 0.792(0.741~0.844) | 0.221 | 0.452 | 0.776 | 0.676 | <0.001 |
Table 3 The predictive value of L3 SMI,SOFA score,APACHEⅡ score and combined variables on the risk of in-hospital mortality in older patients with intra-abdominal sepsis
| 变量 | AUC(95%CI) | 最佳截断值 | 约登指数 | 灵敏度 | 特异度 | P值 |
|---|---|---|---|---|---|---|
| L3 SMI | 0.711(0.650~0.772) | 33.30 cm2/m2 | 0.364 | 0.788 | 0.576 | <0.001 |
| SOFA评分 | 0.740(0.675~0.806) | 5.5分 | 0.455 | 0.647 | 0.808 | <0.001 |
| APACHE Ⅱ评分 | 0.742(0.684~0.801) | 12.5分 | 0.346 | 0.718 | 0.628 | <0.001 |
| L3 SMI联合SOFA评分 | 0.795(0.742~0.847) | 0.336 | 0.468 | 0.600 | 0.868 | <0.001 |
| L3 SMI联合APACHE Ⅱ评分 | 0.792(0.741~0.844) | 0.221 | 0.452 | 0.776 | 0.676 | <0.001 |
| 指标 | 差异 | Z值 | P值 |
|---|---|---|---|
| SOFA评分比L3 SMI | 0.029 | 0.651 | 0.515 |
| L3 SMI联合SOFA评分比L3 SMI | 0.084 | 3.587 | <0.001 |
| L3 SMI联合SOFA评分比SOFA评分 | 0.054 | 2.114 | 0.035 |
| L3 SMI联合SOFA评分比APACHE Ⅱ评分 | 0.052 | 1.577 | 0.115 |
| L3 SMI联合SOFA评分比APACHE Ⅱ评分联合L3 SMI | 0.002 | 0.131 | 0.895 |
| APACHE Ⅱ评分比L3 SMI | 0.031 | 0.722 | 0.470 |
| APACHE Ⅱ评分比SOFA评分 | 0.002 | 0.058 | 0.954 |
| L3 SMI联合APACHE Ⅱ评分比L3 SMI | 0.081 | 3.634 | <0.001 |
| L3 SMI联合APACHE Ⅱ评分比APACHE Ⅱ评分 | 0.050 | 2.075 | 0.038 |
| L3 SMI联合APACHE Ⅱ评分比SOFA评分 | 0.052 | 1.442 | 0.149 |
Table 4 Comparison of the predictive value of L3 SMI,SOFA score,APACHEⅡ score and combined variables on the risk of in-hospital mortality in older patients with intra-abdominal sepsis
| 指标 | 差异 | Z值 | P值 |
|---|---|---|---|
| SOFA评分比L3 SMI | 0.029 | 0.651 | 0.515 |
| L3 SMI联合SOFA评分比L3 SMI | 0.084 | 3.587 | <0.001 |
| L3 SMI联合SOFA评分比SOFA评分 | 0.054 | 2.114 | 0.035 |
| L3 SMI联合SOFA评分比APACHE Ⅱ评分 | 0.052 | 1.577 | 0.115 |
| L3 SMI联合SOFA评分比APACHE Ⅱ评分联合L3 SMI | 0.002 | 0.131 | 0.895 |
| APACHE Ⅱ评分比L3 SMI | 0.031 | 0.722 | 0.470 |
| APACHE Ⅱ评分比SOFA评分 | 0.002 | 0.058 | 0.954 |
| L3 SMI联合APACHE Ⅱ评分比L3 SMI | 0.081 | 3.634 | <0.001 |
| L3 SMI联合APACHE Ⅱ评分比APACHE Ⅱ评分 | 0.050 | 2.075 | 0.038 |
| L3 SMI联合APACHE Ⅱ评分比SOFA评分 | 0.052 | 1.442 | 0.149 |
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
中华医学会外科学分会外科感染与重症医学学组,中国医师协会外科医师分会肠瘘外科医师专业委员会. 中国腹腔感染诊治指南(2019版)[J]. 中国实用外科杂志,2020,40(1):1-16. DOI:10.19538/j.cjps.issn1005-2208.2020.01.01.
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
中国急诊危重症患者肠内营养治疗专家共识组. 中国急诊危重症患者肠内营养治疗专家共识[J]. 中华急诊医学杂志,2022,31(3):281-290. DOI:10.3760/cma.j.issn.1671-0282.2022.03.004.
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
汪颖,王迪芬,付江泉,等. SOFA、qSOFA评分和传统指标对脓毒症预后的判断价值[J]. 中华危重病急救医学,2017,29(8):700-704. DOI:10.3760/cma.j.issn.2095-4352.2017.08.006.
|
| [21] |
|
| [22] |
李平娜,杨宏富,崔秋敏,等. 脓毒症患者细胞因子表达水平及其对预后的影响[J]. 中华危重病急救医学,2023,35(12):1250-1254. DOI:10.3760/cma.j.cn121430-20230818-00660.
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] | |
| [27] |
|
| [28] |
|
| [1] | XU Baichuan, WANG Yan, ZHANG Peng, LI Yiting, LIU Feilai, XIE Yang. Research and Analysis of Screening Tools for Chronic Obstructive Pulmonary Disease Comorbidity Lung Cancer [J]. Chinese General Practice, 2025, 28(30): 3847-3852. |
| [2] | LI Ling, LI Yaping, QIAN Shixing, NIE Jing, LU Chunhua, LI Xia. Research on Influencing Factors and Risk Prediction of Cognitive Function in Community-dwelling Middle-aged and Elderly People [J]. Chinese General Practice, 2025, 28(30): 3773-3778. |
| [3] | XU Jialan, YAN Hong, WEN Jun, ZHOU Zitong, WANG Siyu. Prevalence of Potentially Inappropriate Medication in Older Adults with Cancer: a Meta-analysis [J]. Chinese General Practice, 2025, 28(30): 3815-3822. |
| [4] | SHAO Xiaoying, SHAO Jie, ZHU Yan, SHAO Jinling, SHANG Ling, WU Zhenlian, ZHAO Yu, ZHANG Jiacai. Analysis of the Current Status of Iron Deficiency and Factors Affecting Iron Deficiency Anemia among Children Aged 6-36 Months in Guizhou Province [J]. Chinese General Practice, 2025, 28(27): 3368-3374. |
| [5] | XU Yanpeng, HUANG Pe, ZHANG Pingping, LUO Yan, SHI Xiaoqi, WU Liusong, CHEN Yan, HE Zhixu. Expression of β-Adrenergic Receptors in Acute T-cell Lymphoblastic Leukemia and Its Clinical Significance [J]. Chinese General Practice, 2025, 28(27): 3391-3398. |
| [6] | LI Jiaxin, LIU Zhonghui, XIE Shuo, FU Zhifang, SUN Dan, JIAO Hongmei. Trajectory in Biomarkers of Metabolic and Inflammatory States as Early Predictors of Chronic Critical Illness in Aging Patients [J]. Chinese General Practice, 2025, 28(24): 2993-2999. |
| [7] | YU Wenhua, LI Jianguo, DUAN Wenyan, GAO Xuyan, LI Xiaxia, ZHANG Zilong, ZHANG Li, MA Lina. Reliability and Validity of the Function Impairment Screening Tool among Community-dwelling Older Adults [J]. Chinese General Practice, 2025, 28(24): 3000-3004. |
| [8] | YANG Chen, CHEN Tong, ZHANG Lifang, ZHANG Hongxu, LI Pengfei, ZHANG Xuejuan. Prognostic Impact of Dapagliflozin in Elderly Breast Cancer Survivors with Heart Failure with Preserved Ejection Fraction and Type 2 Diabetes [J]. Chinese General Practice, 2025, 28(24): 3053-3058. |
| [9] | JIANG Shihua, ZHU Zheng, REN Yingying, ZHU Yaolei, WANG Yue, GAO Xibin. Meta Analysis of the Prevalence and Risk Factors of Myopia in Chinese Children and Adolescents [J]. Chinese General Practice, 2025, 28(24): 3043-3052. |
| [10] | ZHOU Qian, WU Xiaomin, WANG Baohua, YAN Ruohan, YU Miao, WU Jing. Study on Nomogram Prediction Model for Risk of Gastric Cancer [J]. Chinese General Practice, 2025, 28(23): 2870-2877. |
| [11] | CHEN Fei, WANG Jinying, YU Haibo, LI Xin, ZHANG Jiajia, SHEN Man, ZHAN Xiaokai, TANG Ran, FAN Sibin, ZHAO Fengyi, ZHANG Tianyu, HUANG Zhongxia. Significance of Elevated Urinary NGAL, TIM-1, VCAM-1 and Activin A in Patients with New Diagnosed Multiple Myeloma [J]. Chinese General Practice, 2025, 28(22): 2740-2749. |
| [12] | ZHAO Xiaoqing, GUO Tongtong, ZHANG Xinyi, LI Linhong, ZHANG Ya, JI Lihong, DONG Zhiwei, GAO Qianqian, CAI Weiqing, ZHENG Wengui, JING Qi. Construction and Validation of a Risk Prediction Model for Cognitive Impairment in Community-dwelling Older Adults [J]. Chinese General Practice, 2025, 28(22): 2776-2783. |
| [13] | SHI Xiaotian, WANG Shan, YANG Huayu, YANG Yifan, LI Xu, MA Qing. Association between Body Mass Index and Mortality among Older Chinese: a Cohort Study [J]. Chinese General Practice, 2025, 28(22): 2791-2797. |
| [14] | LIU Meixia, YIN Jinnian, WU Mei, YANG Xing, ZHOU Quanxiang, YANG Jingyuan. Impact of Body Mass Index on the Association of Triglyceride Glucose Index with Cognitive Function: a Cross-sectional Study in Rural Older Adults in Guizhou Province [J]. Chinese General Practice, 2025, 28(22): 2806-2812. |
| [15] | GUO Shengteng, ZHANG Fenfen, WAN Di, YU Dongmei, WANG Qinghua. Risk Factors for Severe Acute Pancreatitis Complicated with Acute Lung Injury: a Meta-analysis [J]. Chinese General Practice, 2025, 28(20): 2546-2554. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||