

Chinese General Practice ›› 2024, Vol. 27 ›› Issue (32): 3987-3992.DOI: 10.12114/j.issn.1007-9572.2024.0047
• Original Research • Previous Articles Next Articles
Received:2024-03-10
Revised:2024-05-20
Published:2024-11-15
Online:2024-08-08
Contact:
HU Xiaowen
通讯作者:
胡晓文
作者简介:作者贡献:
吕广瑜进行文章的构思与设计,结果分析与解释,统计学处理及论文撰写;吕广瑜和孙宛君进行数据收集与整理;周倩倩、陈先梦、胡晓文进行研究的实施,论文的修订;刘雪晗负责论文统计学方法的设计及可行性分析;胡晓文对研究设计、质量控制进行指导和论文修改,对文章整体监督管理。
基金资助:CLC Number:
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.chinagp.net/EN/10.12114/j.issn.1007-9572.2024.0047
| 年份 | 例数 | 曾误诊为肺炎 |
|---|---|---|
| 2017年 | 6 | 6(100.0) |
| 2018年 | 12 | 10(83.3) |
| 2019年 | 27 | 20(74.1) |
| 2020年 | 7 | 5(71.4) |
| 2021年 | 19 | 12(63.2) |
| 2022年 | 12 | 8(66.7) |
| 2023年 | 18 | 9(50.0) |
| χ2趋势值 | 6.672 | |
| P值 | 0.010 |
Table 1 The proportion of patients with pulmonary infarction secondary to intermediate and high-risk pulmonary embolism misdiagnosed as pneumonia from 2017 to 2023
| 年份 | 例数 | 曾误诊为肺炎 |
|---|---|---|
| 2017年 | 6 | 6(100.0) |
| 2018年 | 12 | 10(83.3) |
| 2019年 | 27 | 20(74.1) |
| 2020年 | 7 | 5(71.4) |
| 2021年 | 19 | 12(63.2) |
| 2022年 | 12 | 8(66.7) |
| 2023年 | 18 | 9(50.0) |
| χ2趋势值 | 6.672 | |
| P值 | 0.010 |
| 组别 | 例数 | 性别(男/女) | 年龄[M(P25,P75),岁] | 吸烟史[例(%)] | 饮酒史[例(%)] | 发热[例(%)] | 咳嗽[例(%)] | 胸痛[例(%)] | 呼吸困难[例(%)] | 咯血[例(%)] |
|---|---|---|---|---|---|---|---|---|---|---|
| 对照组 | 31 | 20/11 | 53.0(42.0,66.0) | 4(12.9) | 2(6.5) | 6(19.4) | 14(45.2) | 6(19.4) | 24(77.4) | 10(32.3) |
| 误诊组 | 70 | 43/27 | 67.5(56.5,73.0) | 14(20.0) | 12(17.1) | 40(57.1) | 38(54.3) | 30(42.9) | 30(42.9) | 15(21.4) |
| χ2(Z)值 | 0.087 | -3.488a | — | — | 12.370 | 0.716 | 5.174 | 10.316 | 1.353 | |
| P值 | 0.768 | <0.001 | 0.574 | 0.216 | <0.001 | 0.397 | 0.023 | 0.001 | 0.245 | |
| 组别 | 单侧下肢肿痛[例(%)] | 白细胞计数[M(P25,P75),×109/L] | 肌钙蛋白[M(P25,P75),ng/mL] | D-二聚体[M(P25,P75),mg/L] | 氨基末端脑利钠肽前体[M(P25,P75),ng/L] | 病灶梗死位置[例(%)] | ||||
| 左侧 | 右侧 | 双侧 | ||||||||
| 对照组 | 8(25.8) | 8.47(6.27,12.24) | 0.02(0.01,0.10) | 4.16(2.53,7.78) | 969.00(100.00,4 376.00) | 16(51.6) | 12(38.7) | 3(9.7) | ||
| 误诊组 | 19(27.1) | 8.59(6.38,11.35) | 0.03(0.01,0.12) | 6.68(3.39,18.47) | 572.00(237.00,1 897.00) | 20(28.6) | 40(57.1) | 10(14.3) | ||
| χ2(Z)值 | 0.020 | -0.162a | -0.418a | -1.900a | -0.060a | 4.973 | ||||
| P值 | 0.889 | 0.871 | 0.676 | 0.057 | 0.952 | 0.083 | ||||
| 组别 | 病灶肺叶分布[例(%)] | 梗死病灶影像学征象[例(%)] | 预后情况[例(%)] | |||||||
| 上叶 | 中叶 | 下叶 | 楔形影 | 中央透亮影征 | 血管征 | 充气征 | 死亡 | 良好 | ||
| 对照组 | 6(19.3) | 2(6.4) | 25(80.6) | 22(71.0) | 18(58.1) | 8(25.8) | 8(25.8) | 1(3.2) | 30(96.8) | |
| 误诊组 | 13(18.6) | 7(10.0) | 56(80.0) | 32(45.7) | 41(58.6) | 30(42.9) | 15(21.4) | 4(5.7) | 66(94.3) | |
| χ2(Z)值 | 0.009 | — | 0.006 | 5.507 | 0.002 | 2.662 | 0.234 | — | ||
| P值 | 0.926 | 0.718 | 0.940 | 0.019 | 0.962 | 0.103 | 0.628 | 1.000 | ||
Table 2 Comparison of clinical characteristics of patients between misdiagnosis group and control group
| 组别 | 例数 | 性别(男/女) | 年龄[M(P25,P75),岁] | 吸烟史[例(%)] | 饮酒史[例(%)] | 发热[例(%)] | 咳嗽[例(%)] | 胸痛[例(%)] | 呼吸困难[例(%)] | 咯血[例(%)] |
|---|---|---|---|---|---|---|---|---|---|---|
| 对照组 | 31 | 20/11 | 53.0(42.0,66.0) | 4(12.9) | 2(6.5) | 6(19.4) | 14(45.2) | 6(19.4) | 24(77.4) | 10(32.3) |
| 误诊组 | 70 | 43/27 | 67.5(56.5,73.0) | 14(20.0) | 12(17.1) | 40(57.1) | 38(54.3) | 30(42.9) | 30(42.9) | 15(21.4) |
| χ2(Z)值 | 0.087 | -3.488a | — | — | 12.370 | 0.716 | 5.174 | 10.316 | 1.353 | |
| P值 | 0.768 | <0.001 | 0.574 | 0.216 | <0.001 | 0.397 | 0.023 | 0.001 | 0.245 | |
| 组别 | 单侧下肢肿痛[例(%)] | 白细胞计数[M(P25,P75),×109/L] | 肌钙蛋白[M(P25,P75),ng/mL] | D-二聚体[M(P25,P75),mg/L] | 氨基末端脑利钠肽前体[M(P25,P75),ng/L] | 病灶梗死位置[例(%)] | ||||
| 左侧 | 右侧 | 双侧 | ||||||||
| 对照组 | 8(25.8) | 8.47(6.27,12.24) | 0.02(0.01,0.10) | 4.16(2.53,7.78) | 969.00(100.00,4 376.00) | 16(51.6) | 12(38.7) | 3(9.7) | ||
| 误诊组 | 19(27.1) | 8.59(6.38,11.35) | 0.03(0.01,0.12) | 6.68(3.39,18.47) | 572.00(237.00,1 897.00) | 20(28.6) | 40(57.1) | 10(14.3) | ||
| χ2(Z)值 | 0.020 | -0.162a | -0.418a | -1.900a | -0.060a | 4.973 | ||||
| P值 | 0.889 | 0.871 | 0.676 | 0.057 | 0.952 | 0.083 | ||||
| 组别 | 病灶肺叶分布[例(%)] | 梗死病灶影像学征象[例(%)] | 预后情况[例(%)] | |||||||
| 上叶 | 中叶 | 下叶 | 楔形影 | 中央透亮影征 | 血管征 | 充气征 | 死亡 | 良好 | ||
| 对照组 | 6(19.3) | 2(6.4) | 25(80.6) | 22(71.0) | 18(58.1) | 8(25.8) | 8(25.8) | 1(3.2) | 30(96.8) | |
| 误诊组 | 13(18.6) | 7(10.0) | 56(80.0) | 32(45.7) | 41(58.6) | 30(42.9) | 15(21.4) | 4(5.7) | 66(94.3) | |
| χ2(Z)值 | 0.009 | — | 0.006 | 5.507 | 0.002 | 2.662 | 0.234 | — | ||
| P值 | 0.926 | 0.718 | 0.940 | 0.019 | 0.962 | 0.103 | 0.628 | 1.000 | ||
| 变量 | β | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 常量 | -2.850 | 0.748 | 14.528 | <0.001 | — |
| 年龄≥60岁 | 2.905 | 0.730 | 15.860 | <0.001 | 18.271(4.373~76.339) |
| 发热 | 2.777 | 0.778 | 12.756 | <0.001 | 16.073(3.510~73.786) |
| 胸痛 | 1.896 | 0.737 | 6.620 | 0.010 | 6.660(1.571~28.233) |
| 不伴有呼吸困难 | 2.063 | 0.687 | 9.027 | 0.003 | 7.783(2.049~30.249) |
Table 3 Multivariate binary Logistic regression analysis of risk factors related to pulmonary infarction secondary to intermediate and high-risk pulmonary embolism misdiagnosed as pneumonia
| 变量 | β | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 常量 | -2.850 | 0.748 | 14.528 | <0.001 | — |
| 年龄≥60岁 | 2.905 | 0.730 | 15.860 | <0.001 | 18.271(4.373~76.339) |
| 发热 | 2.777 | 0.778 | 12.756 | <0.001 | 16.073(3.510~73.786) |
| 胸痛 | 1.896 | 0.737 | 6.620 | 0.010 | 6.660(1.571~28.233) |
| 不伴有呼吸困难 | 2.063 | 0.687 | 9.027 | 0.003 | 7.783(2.049~30.249) |
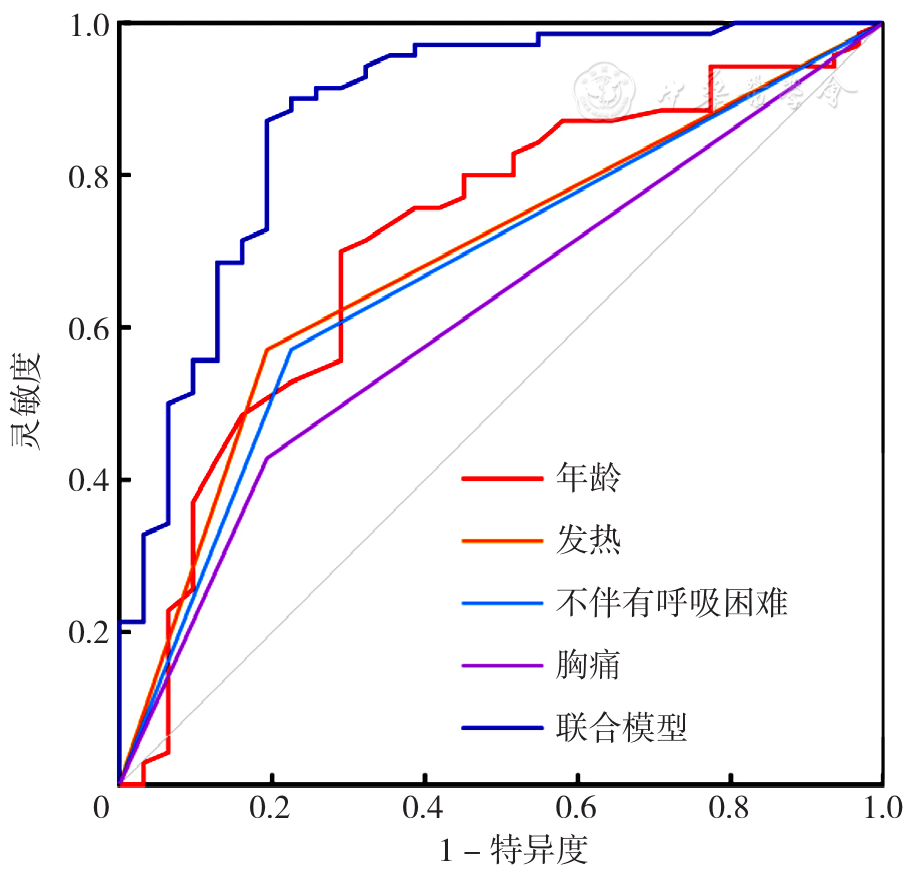
Figure 2 ROC curve of individual and combined forecasts of pulmonary infarction secondary to intermediate and high-risk pulmonary embolism misdiagnosed as pneumonia
| 变量 | AUC | 95%CI | P值 | 标准误 | 灵敏度 | 特异度 |
|---|---|---|---|---|---|---|
| 年龄≥60岁 | 0.718 | 0.608~0.829 | <0.001 | 0.056 | 0.700 | 0.710 |
| 发热 | 0.689 | 0.580~0.798 | 0.003 | 0.056 | 0.571 | 0.806 |
| 胸痛 | 0.618 | 0.503~0.732 | 0.060 | 0.059 | ||
| 不伴有呼吸困难 | 0.673 | 0.561~0.784 | <0.001 | 0.057 | 0.571 | 0.774 |
Table 4 The predictive value of age,fever,absence of dyspnea,and combined models for misdiagnosis
| 变量 | AUC | 95%CI | P值 | 标准误 | 灵敏度 | 特异度 |
|---|---|---|---|---|---|---|
| 年龄≥60岁 | 0.718 | 0.608~0.829 | <0.001 | 0.056 | 0.700 | 0.710 |
| 发热 | 0.689 | 0.580~0.798 | 0.003 | 0.056 | 0.571 | 0.806 |
| 胸痛 | 0.618 | 0.503~0.732 | 0.060 | 0.059 | ||
| 不伴有呼吸困难 | 0.673 | 0.561~0.784 | <0.001 | 0.057 | 0.571 | 0.774 |
| 变量 | β | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 常量 | -6.624 | 1.625 | 16.616 | <0.001 | — |
| 年龄≥60岁 | 0.095 | 0.023 | 16.700 | <0.001 | 1.100(1.051~1.151) |
| 发热 | 2.510 | 0.684 | 13.458 | <0.001 | 12.307(3.219~47.053) |
| 不伴有呼吸困难 | 2.683 | 0.757 | 12.572 | <0.001 | 14.627(3.320~64.450) |
Table 5 Multivariate binary Logistic regression analysis of age,fever and absence of dyspnea as influencing factors of misdiagnosis of secondary PI as pneumonia in middle and high risk PE
| 变量 | β | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 常量 | -6.624 | 1.625 | 16.616 | <0.001 | — |
| 年龄≥60岁 | 0.095 | 0.023 | 16.700 | <0.001 | 1.100(1.051~1.151) |
| 发热 | 2.510 | 0.684 | 13.458 | <0.001 | 12.307(3.219~47.053) |
| 不伴有呼吸困难 | 2.683 | 0.757 | 12.572 | <0.001 | 14.627(3.320~64.450) |
| [1] |
|
| [2] |
中华医学会呼吸病学分会肺栓塞与肺血管病学组,中国医师协会呼吸医师分会肺栓塞与肺血管病工作委员会,全国肺栓塞与肺血管病防治协作组. 肺血栓栓塞症诊治与预防指南[J]. 中华医学杂志,2018,98(14):1060-1087.
|
| [3] |
|
| [4] |
|
| [5] |
孙宛君. 119例肺栓塞继发肺梗死临床分析[D]. 合肥:安徽医科大学,2021.
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
路明,陈亚红,姚中强,等. 发热、胸痛、咯血、双肺多发实变影[J]. 中华结核和呼吸杂志,2016,39(12):992-994. DOI:10.3760/cma.j.issn.1001-0939.2016.12.023.
|
| [14] |
牟向东,李桂莲,张建华,等. 发热、咯血、胸痛、左下肺阴影[J]. 中华结核和呼吸杂志,2012,35(9):710-711.
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
宋华峰,吴妹英,张建平,等. 血清蛋白指标在构建肺结核治疗预后评估的早期预测模型中的应用价值[J]. 中华结核和呼吸杂志,2023,46(7):664-673. DOI:10.3760/cma.j.cn112147-20221021-00836.
|
| [23] |
|
| [24] |
|
| [1] | ZHANG Long, LI Jianping. Establishment and Promotion of a Dyslipidemia Management and Control System Grounded on Hierarchical Medical Treatment [J]. Chinese General Practice, 2024, 27(36): 4493-4497. |
| [2] | ZHOU Zhensen, HUANG Yan, CHENG Siwei, ZHANG Xiaoyu, ZHANG Xiaoyu, SUN Ting, YANG Xianjun, XIE Hui, MA Zuchang. Construction and Validation of a Screening Model for Early Atherosclerosis Risk in the Aorta [J]. Chinese General Practice, 2024, 27(33): 4147-4154. |
| [3] | WANG Wuchao, LIU Siqi, LIU Qianqian, ZHU Jihong. Clinical Characteristics of Acute Pulmonary Embolism Complicated with Thrombocytopenia: a Retrospective Study [J]. Chinese General Practice, 2024, 27(27): 3372-3377. |
| [4] | LI Qiuling, TANG Wenwu, YU Yiwen, DENG Huan, YANG Xiaohua, CHEN Xiaoxia, JI Yifei. Establishment and Verification of Risk Prediction Model for Silent Brain Infarction in Maintenance Hemodialysis Patients: a Multicenter Study [J]. Chinese General Practice, 2024, 27(26): 3232-3239. |
| [5] | ZHANG Lan, ZHANG Ruihua, WU Xuelian, YANG Yan, DUAN Guimin, ZHAO Daren. Equity Analysis and Demand Prediction of General Practitioner Resource Allocation in Western China [J]. Chinese General Practice, 2024, 27(25): 3171-3177. |
| [6] | JIANG Qixia, XIE Haoting, WANG Huajun, LI Xiuyun, ZHU Yuling, WANG Yaling, MIN Yan, WANG Ke. Effectiveness Analysis of Two Incontinence Care Plans Based on Guidelines for Elderly COVID-19 Patients with Incontinence [J]. Chinese General Practice, 2024, 27(18): 2212-2217. |
| [7] | MIAO Lipeng, REN Kehao, LI Mengdie, LYU Juncheng. Trend Analysis and Prediction of Cardiovascular Disease Mortality in China from 2009 to 2021 [J]. Chinese General Practice, 2024, 27(18): 2260-2264. |
| [8] | GAO Ying, XU Xinyi, LIU Yang, YANG Xiaokun. Research on the Development of Atherosclerotic Cardiovascular Disease Prediction Model for the Elderly Based on TCM Constitution [J]. Chinese General Practice, 2024, 27(15): 1878-1885. |
| [9] | LIU Caixia, AN Tingting, LIU Jing, LI Xiangyang, JIN Jie, XU Lanjuan. Prognostic Value of IMPACT and CRASH Models in the Assessment of Patients with Traumatic Brain Injury: a Comparative Study [J]. Chinese General Practice, 2024, 27(15): 1843-1849. |
| [10] | YANG Shuo, LIU Xinying, WANG Huizhe, LI Huanmin, LI Xinmin. Risk Factors for Severe Mycoplasma Pneumoniae Pneumonia in Children: a Meta-analysis [J]. Chinese General Practice, 2024, 27(14): 1750-1760. |
| [11] | ZHONG Jinjia, LI Wentao, HUANG Yafang, WU Hao. Design Features and Methodological Quality of Researches about Prediction Models Based on Machine Learning in Primary Care: a Scoping Review [J]. Chinese General Practice, 2024, 27(10): 1271-1276. |
| [12] | ZENG Lingcong, ZHANG Longju, ZHOU Ling, ZHANG Wei, DAI Meng, HUANG Yin, HUANG Yi. Analysis of the Predictive Value of 4-level Clinical Pretest Probability Score in Elderly Patients with Acute Pulmonary Embolism [J]. Chinese General Practice, 2024, 27(09): 1062-1067. |
| [13] | HAN Junjie, WU Di, CHEN Zhisheng, XIAO Yang, SEN Gan. A Nomogram Prediction Model and Validation Study on the Risk of Complicated Diabetic Nephropathy in Type 2 Diabetes Patients [J]. Chinese General Practice, 2024, 27(09): 1054-1061. |
| [14] | ZOU Qiong, WU Xi, ZHANG Yang, WAN Yi, CHEN Changsheng. Prediction of Type 2 Diabetic Nephropathy Based on BP Neural Network Optimized by Sparrow Search Algorithm [J]. Chinese General Practice, 2024, 27(08): 961-970. |
| [15] | WANG Minghang, HAN Weihong, BI Lichan, YANG Jiang, LI Jiansheng. Evaluation Study of Traditional Chinese Medicine Syndrome Differentiation Therapy on the Quality of Life and Efficacy Satisfaction in Elderly Community-acquired Pneumonia Patients after Discharge [J]. Chinese General Practice, 2024, 27(08): 1001-1007. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||