

Chinese General Practice ›› 2022, Vol. 25 ›› Issue (23): 2874-2880.DOI: 10.12114/j.issn.1007-9572.2022.0234
Special Issue: 骨健康最新文章合辑; 营养最新文章合辑; 老年问题最新文章合辑
• Article • Previous Articles Next Articles
Received:2021-12-24
Revised:2022-04-20
Published:2022-08-15
Online:2022-06-02
Contact:
Limin LIU
About author:
通讯作者:
刘利民
作者简介:基金资助:
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.chinagp.net/EN/10.12114/j.issn.1007-9572.2022.0234
| 一般资料 | 死亡组(n=47) | 存活组(n=352) | 检验统计量值 | P值 | |
|---|---|---|---|---|---|
| 性别〔n(%)〕 | 1.809a | 0.179 | |||
| 男 | 20(42.55) | 115(32.67) | |||
| 女 | 27(57.45) | 237(67.33) | |||
| 年龄( | 82.6±7.5 | 77.2±8.6 | 4.101b | <0.001 | |
| 骨折部位〔n(%)〕 | 1.481a | 0.224 | |||
| 股骨颈骨折 | 16(34.04) | 153(43.47) | |||
| 转子间骨折 | 31(65.96) | 199(56.53) | |||
| 合并内科疾病〔n(%)〕 | |||||
| 原发性高血压病 | 24(51.06) | 202(57.39) | 0.905a | 0.342 | |
| 2型糖尿病 | 12(25.53) | 109(30.97) | 1.016a | 0.314 | |
| 陈旧性脑梗死 | 16(34.04) | 78(22.16) | 3.097a | 0.078 | |
| 血红蛋白〔M(P25,P75),g/L〕 | 108(96,119) | 122(107,133) | -3.727 | <0.001 | |
| 白蛋白〔M(P25,P75),g/L〕 | 33.58(31.62,38.00) | 37.18(34.77,40.00) | -3.770 | <0.001 | |
| 肌酐〔M(P25,P75),μmol/L〕 | 78(59,104) | 60(50,73) | -4.113 | <0.001 | |
| 前白蛋白〔M(P25,P75),g/L〕 | 146(103,198) | 170(138,208) | -2.665 | 0.008 | |
| D-二聚体〔M(P25,P75),μg/L〕 | 1.25(0.56,3.17) | 1.20(0.37,2.57) | -1.130 | 0.259 | |
| 术前CONUT评分〔M(P25,P75),分〕 | 4(2,6) | 3(2,4) | -4.076 | <0.001 | |
| GNRI( | 121.40±16.09 | 126.14±15.04 | -2.013b | 0.045 | |
| NLR〔M(P25,P75),μg/L〕 | 5.72(3.96,9.70) | 4.89(3.55,6.96) | -2.472 | 0.013 | |
Table 1 Comparison of general data between the deceased and survived elderly patients with hip fracture
| 一般资料 | 死亡组(n=47) | 存活组(n=352) | 检验统计量值 | P值 | |
|---|---|---|---|---|---|
| 性别〔n(%)〕 | 1.809a | 0.179 | |||
| 男 | 20(42.55) | 115(32.67) | |||
| 女 | 27(57.45) | 237(67.33) | |||
| 年龄( | 82.6±7.5 | 77.2±8.6 | 4.101b | <0.001 | |
| 骨折部位〔n(%)〕 | 1.481a | 0.224 | |||
| 股骨颈骨折 | 16(34.04) | 153(43.47) | |||
| 转子间骨折 | 31(65.96) | 199(56.53) | |||
| 合并内科疾病〔n(%)〕 | |||||
| 原发性高血压病 | 24(51.06) | 202(57.39) | 0.905a | 0.342 | |
| 2型糖尿病 | 12(25.53) | 109(30.97) | 1.016a | 0.314 | |
| 陈旧性脑梗死 | 16(34.04) | 78(22.16) | 3.097a | 0.078 | |
| 血红蛋白〔M(P25,P75),g/L〕 | 108(96,119) | 122(107,133) | -3.727 | <0.001 | |
| 白蛋白〔M(P25,P75),g/L〕 | 33.58(31.62,38.00) | 37.18(34.77,40.00) | -3.770 | <0.001 | |
| 肌酐〔M(P25,P75),μmol/L〕 | 78(59,104) | 60(50,73) | -4.113 | <0.001 | |
| 前白蛋白〔M(P25,P75),g/L〕 | 146(103,198) | 170(138,208) | -2.665 | 0.008 | |
| D-二聚体〔M(P25,P75),μg/L〕 | 1.25(0.56,3.17) | 1.20(0.37,2.57) | -1.130 | 0.259 | |
| 术前CONUT评分〔M(P25,P75),分〕 | 4(2,6) | 3(2,4) | -4.076 | <0.001 | |
| GNRI( | 121.40±16.09 | 126.14±15.04 | -2.013b | 0.045 | |
| NLR〔M(P25,P75),μg/L〕 | 5.72(3.96,9.70) | 4.89(3.55,6.96) | -2.472 | 0.013 | |
| 因素 | β | SE | Wald χ2值 | P值 | OR值 | 95%CI |
|---|---|---|---|---|---|---|
| 年龄 | 0.089 | 0.025 | 12.403 | 0.001 | 1.093 | (1.040,1.148) |
| 陈旧性脑梗死 | -1.041 | 0.376 | 7.684 | 0.006 | 0.353 | (0.169,0.737) |
| 血红蛋白 | -0.003 | 0.009 | 0.100 | 0.751 | 0.997 | (0.978,1.013) |
| 白蛋白 | -0.060 | 0.054 | 1.260 | 0.262 | 0.941 | (0.847,1.046) |
| 肌酐 | 0.006 | 0.002 | 7.993 | 0.005 | 1.006 | (1.002,1.010) |
| 前白蛋白 | 0.002 | 0.004 | 0.163 | 0.687 | 1.002 | (0.993,1.010) |
| 术前CONUT评分 | 0.232 | 0.116 | 4.011 | 0.045 | 1.261 | (1.005,1.583) |
| GNRI | 0.012 | 0.013 | 0.826 | 0.363 | 1.012 | (0.986,1.039) |
| NLR | 0.048 | 0.023 | 4.382 | 0.036 | 1.049 | (1.003,1.098) |
Table 2 Multivariate Logistic regression analysis of the influencing factors of 1-year postoperative mortality in elderly patients with hip fracture
| 因素 | β | SE | Wald χ2值 | P值 | OR值 | 95%CI |
|---|---|---|---|---|---|---|
| 年龄 | 0.089 | 0.025 | 12.403 | 0.001 | 1.093 | (1.040,1.148) |
| 陈旧性脑梗死 | -1.041 | 0.376 | 7.684 | 0.006 | 0.353 | (0.169,0.737) |
| 血红蛋白 | -0.003 | 0.009 | 0.100 | 0.751 | 0.997 | (0.978,1.013) |
| 白蛋白 | -0.060 | 0.054 | 1.260 | 0.262 | 0.941 | (0.847,1.046) |
| 肌酐 | 0.006 | 0.002 | 7.993 | 0.005 | 1.006 | (1.002,1.010) |
| 前白蛋白 | 0.002 | 0.004 | 0.163 | 0.687 | 1.002 | (0.993,1.010) |
| 术前CONUT评分 | 0.232 | 0.116 | 4.011 | 0.045 | 1.261 | (1.005,1.583) |
| GNRI | 0.012 | 0.013 | 0.826 | 0.363 | 1.012 | (0.986,1.039) |
| NLR | 0.048 | 0.023 | 4.382 | 0.036 | 1.049 | (1.003,1.098) |
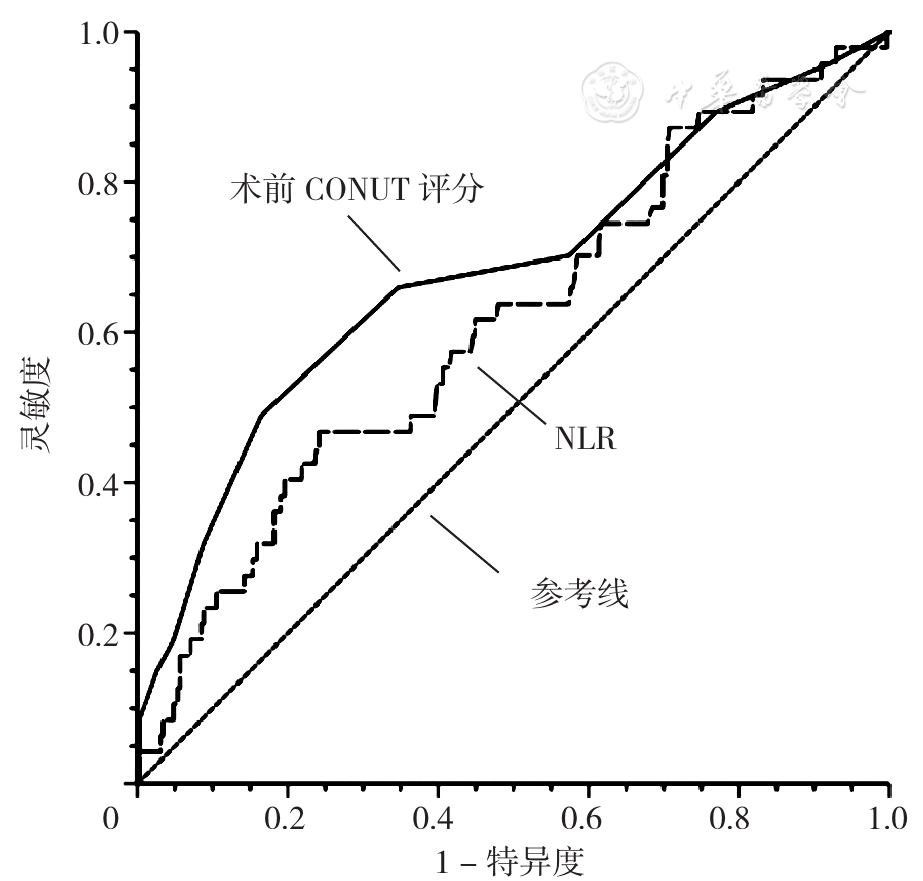
Figure 1 ROC curves of the preoperative CONUT score and neutrophil-to-lymphocyte ratio predicting 1-year postoperative mortality in elderly patients with hip fracture
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
张新玉,安帅,黄江,等. 老年人髋部骨折术后1年内死亡的危险因素研究[J]. 中国全科医学,2018,21(10):1198-1202. DOI:10.3969/j.issn.1007-9572.2018.10.011.
|
| [7] |
赵珅,黄峰,林榕波. 控制营养状态评分评估根治性胃癌切除术患者预后的临床价值[J]. 检验医学与临床,2020,17(4):444-446,451. DOI:10.3969/j.issn.1672-9455.2020.04.004.
|
| [8] |
|
| [9] |
陈洁琼,杨洋,谢楚珊,等. 营养控制状态评分对老年急性心肌梗死患者行急诊PCI术后1年内主要不良心血管事件的预测价值[J]. 现代消化及介入诊疗,2020,25(8):1080-1083. DOI:10.3969/j.issn.1672-2159.2020.08.021.
|
| [10] |
庄宸麟,余惠珍,余鹏,等. 控制营养状态评分与老年心力衰竭患者营养状况及临床指标的相关性研究[J]. 中外医疗,2021,40(5):4-6. DOI:10.16662/j.cnki.1674-0742.2021.05.004.
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
赵改,谢杰,刘飞,等. 术前血C反应蛋白与白蛋白比值、老年营养风险指数在老年髋部骨折患者预后评估中的价值[J]. 东南大学学报:医学版,2021,40(1):103-107. DOI:10.3969/j.issn.1671-6264.2021.01.020.
|
| [15] |
赵珅,黄峰,林榕波. 控制营养状态评分评估根治性胃癌切除术患者预后的临床价值[J]. 检验医学与临床,2020,17(4):444-446,451. DOI:10.3969/j.issn.1672-9455.2020.04.004.
|
| [16] |
蔡郁,陈小波,朱文清,等. 血清中血管内皮生长因子和血小板源性生长因子与胫腓骨骨折患者骨折愈合及关节功能的关系[J]. 中国卫生检验杂志,2019,29(9):1116-1118.
|
| [17] |
|
| [18] |
|
| [19] |
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
黄松涛,陈文辉,龙治强. 老年髋部骨折患者入院时中性粒细胞/淋巴细胞比值与术后病死率的相关性分析[J]. 中国医师杂志,2020,22(11):1724-1727. DOI:10.3760/cma.j.cn431274-20190818-00962.
|
| [24] |
徐晓婷,张强,杨丽红,等. 中性粒细胞与淋巴细胞比值联合全球急性冠状动脉事件注册研究评分与急性冠脉综合征患者预后的相关性分析[J]. 中国全科医学,2019,22(11):1302-1306. DOI:10.12114/j.issn.1007-9572.2018.00.260.
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
张新玉,安帅,刘利民. 老年髋部骨折术后患者中长期的生活能力水平及其影响因素[J]. 中国医刊,2018,53(1):48-50. DOI:10.3969/j.issn.1008-1070.2018.01.014.
|
| [30] |
钱采韻. 老年脑梗死与认知功能障碍[J]. 实用老年医学,2006,20(4):221-223.
|
| [31] |
|
| [32] |
|
| [33] |
|
| [34] |
|
| [35] |
|
| [36] |
|
| [37] |
唐梦君,丁叔波,胡望远. 老年营养风险指数在行放射治疗高龄食管癌患者预后评估中的价值[J]. 中国医药导报,2020,17(6):62-65.
|
| [38] |
栗志磊,许业传,王梦宇. 老年人营养风险指数对老年肝癌切除术患者术后并发症的预测价值[J]. 安徽医学,2020,41(6):653-656. DOI:10.3969/j.issn.1000-0399.2020.06.010.
|
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||