| [1] |
FRIEDMAN S L, NEUSCHWANDER-TETRI B A, RINELLA M,et al. Mechanisms of NAFLD development and therapeutic strategies[J]. Nat Med, 2018, 24(7):908-922. DOI: 10.1038/s41591-018-0104-9.
|
| [2] |
ITO T, ISHIGAMI M, ISHIZU Y,et al. Utility and limitations of noninvasive fibrosis markers for predicting prognosis in biopsy-proven Japanese non-alcoholic fatty liver disease patients[J]. J Gastroenterol Hepatol, 2019, 34(1):207-214. DOI: 10.1111/jgh.14448.
|
| [3] |
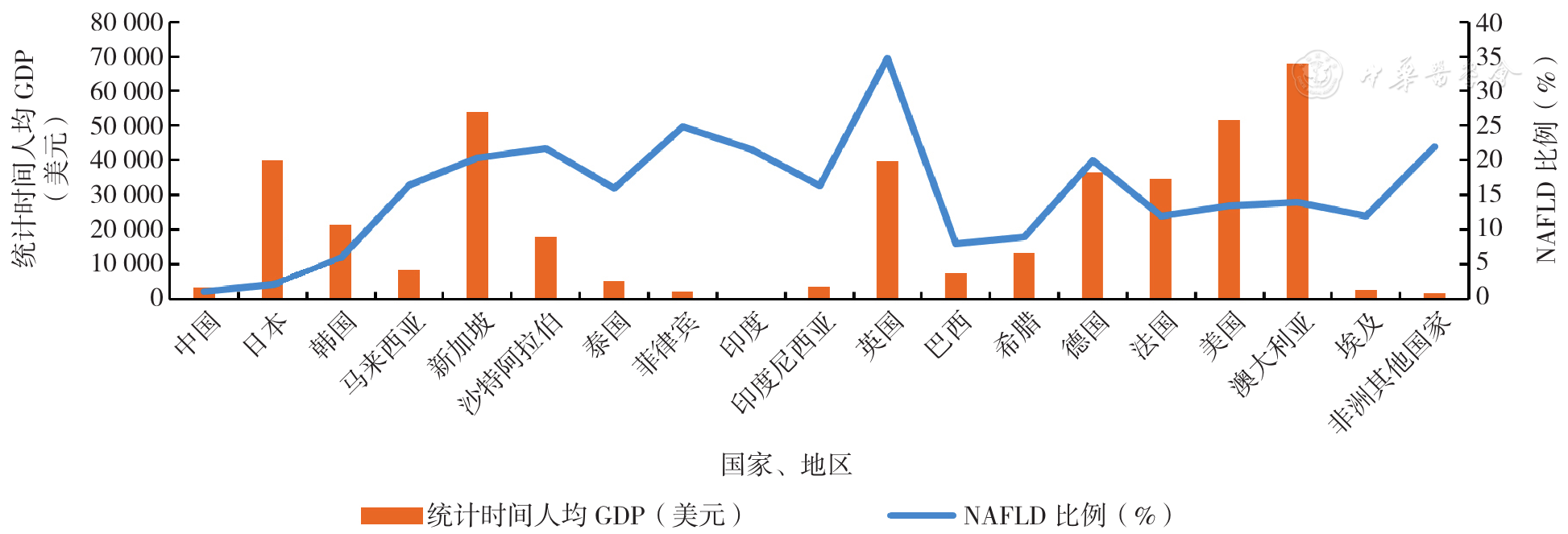
HUANG D Q, EL-SERAG H B, LOOMBA R. Global epidemiology of NAFLD-related HCC:trends,predictions,risk factors and prevention[J]. Nat Rev Gastroenterol Hepatol, 2021, 18(4):223-238. DOI: 10.1038/s41575-020-00381-6.
|
| [4] |
ORCI L A, SANDUZZI-ZAMPARELLI M, CABALLOL B,et al. Incidence of hepatocellular carcinoma in patients with nonalcoholic fatty liver disease:a systematic review,meta-analysis,and meta-regression[J]. Clin Gastroenterol Hepatol, 2022, 20(2):283-292.e10. DOI: 10.1016/j.cgh.2021.05.002.
|
| [5] |
KAYA E D, YILMAZ Y. Metabolic-associated fatty liver disease(MAFLD):a multi-systemic disease beyond the liver[J]. J Clin Transl Hepatol, 2022, 10(2):329-338. DOI: 10.14218/JCTH.2021.00178.
|
| [6] |
YE Q, ZOU B Y, YEO Y H,et al. Global prevalence,incidence,and outcomes of non-obese or lean non-alcoholic fatty liver disease:a systematic review and meta-analysis[J]. Lancet Gastroenterol Hepatol, 2020, 5(8):739-752. DOI: 10.1016/S2468-1253(20)30077-7.
|
| [7] |
RIAZI K, AZHARI H, CHARETTE J H,et al. The prevalence and incidence of NAFLD worldwide:a systematic review and meta-analysis[J]. Lancet Gastroenterol Hepatol, 2022, 7(9):851-861. DOI: 10.1016/S2468-1253(22)00165-0.
|
| [8] |
LONARDO A, NASCIMBENI F, BALLESTRI S,et al. Sex differences in nonalcoholic fatty liver disease:state of the art and identification of research gaps[J]. Hepatology, 2019, 70(4):1457-1469. DOI: 10.1002/hep.30626.
|
| [9] |
ESTES C, ANSTEE Q M, ARIAS-LOSTE M T,et al. Modeling NAFLD disease burden in China,France,Germany,Italy,Japan,Spain,United Kingdom,and United States for the period 2016-2030[J]. J Hepatol, 2018, 69(4):896-904. DOI: 10.1016/j.jhep.2018.05.036.
|
| [10] |
YOUNOSSI Z M, GOLABI P, PAIK J M,et al. The global epidemiology of nonalcoholic fatty liver disease(NAFLD)and nonalcoholic steatohepatitis(NASH):a systematic review[J]. Hepatology, 2023, 77(4):1335-1347. DOI: 10.1097/HEP.0000000000000004.
|
| [11] |
ZHOU J H, ZHOU F, WANG W X,et al. Epidemiological features of NAFLD from 1999 to 2018 in China[J]. Hepatology, 2020, 71(5):1851-1864. DOI: 10.1002/hep.31150.
|
| [12] |
PARK J W, CHEN M S, COLOMBO M,et al. Global patterns of hepatocellular carcinoma management from diagnosis to death:the BRIDGE Study[J]. Liver Int, 2015, 35(9):2155-2166. DOI: 10.1111/liv.12818.
|
| [13] |
TOKUSHIGE K, HASHIMOTO E, HORIE Y,et al. Hepatocellular carcinoma in Japanese patients with nonalcoholic fatty liver disease,alcoholic liver disease,and chronic liver disease of unknown etiology:report of the nationwide survey[J]. J Gastroenterol, 2011, 46(10):1230-1237. DOI: 10.1007/s00535-011-0431-9.
|
| [14] |
GOH K L, RAZLAN H, HARTONO J L,et al. Liver cancer in Malaysia:epidemiology and clinical presentation in a multiracial Asian population[J]. J Dig Dis, 2015, 16(3):152-158. DOI: 10.1111/1751-2980.12223.
|
| [15] |
LIEW Z H, GOH G B, HAO Y,et al. Comparison of hepatocellular carcinoma in patients with cryptogenic versus hepatitis B etiology:a study of 1079 cases over 3 decades[J]. Dig Dis Sci, 2019, 64(2):585-590. DOI: 10.1007/s10620-018-5331-x.
|
| [16] |
ALJUMAH A A, KURIRY H, ALZUNAITAN M,et al. Clinical presentation,risk factors,and treatment modalities of hepatocellular carcinoma:a single tertiary care center experience[J]. Gastroenterol Res Pract, 2016, 2016:1989045. DOI: 10.1155/2016/1989045.
|
| [17] |
SOMBOON K, SIRAMOLPIWAT S, VILAICHONE R K. Epidemiology and survival of hepatocellular carcinoma in the central region of Thailand[J]. Asian Pac J Cancer Prev, 2014, 15(8):3567-3570. DOI: 10.7314/apjcp.2014.15.8.3567.
|
| [18] |
YUEN M F, HOU J L, CHUTAPUTTI A,et al. Hepatocellular carcinoma in the Asia Pacific region[J]. J Gastroenterol Hepatol, 2009, 24(3):346-353. DOI: 10.1111/j.1440-1746.2009.05784.x.
|
| [19] |
PAUL S B, CHALAMALASETTY S B, VISHNUBHATLA S,et al. Clinical profile,etiology and therapeutic outcome in 324 hepatocellular carcinoma patients at a tertiary care center in India[J]. Oncology, 2009, 77(3/4):162-171. DOI: 10.1159/000231886.
|
| [20] |
JASIRWAN C O M, HASAN I, SULAIMAN A S,et al. Risk factors of mortality in the patients with hepatocellular carcinoma:a multicenter study in Indonesia[J]. Curr Probl Cancer, 2020, 44(1):100480. DOI: 10.1016/j.currproblcancer.2019.05.003.
|
| [21] |
DYSON J, JAQUES B, CHATTOPADYHAY D,et al. Hepatocellular cancer:the impact of obesity,type 2 diabetes and a multidisciplinary team[J]. J Hepatol, 2014, 60(1):110-117. DOI: 10.1016/j.jhep.2013.08.011.
|
| [22] |
LOPES F D E L, COELHO F F, KRUGER J A,et al. Influence of hepatocellular carcinoma etiology in the survival after resection[J]. Braz Arch Dig Surg, 2016, 29(2):105-108. DOI: 10.1590/0102-6720201600020010.
|
| [23] |
RAPTIS I, KOSKINAS J, EMMANOUIL T,et al. Changing relative roles of hepatitis B and C viruses in the aetiology of hepatocellular carcinoma in Greece. Epidemiological and clinical observations[J]. J Viral Hepat, 2003, 10(6):450-454. DOI: 10.1046/j.1365-2893.2003.00442.x.
|
| [24] |
GANSLMAYER M, HAGEL A, DAUTH W,et al. A large cohort of patients with hepatocellular carcinoma in a single European centre:aetiology and prognosis now and in a historical cohort[J]. Swiss Med Wkly, 2014, 144:w13900. DOI: 10.4414/smw.2014.13900.
|
| [25] |
PAIS R, FARTOUX L, GOUMARD C,et al. Temporal trends,clinical patterns and outcomes of NAFLD-related HCC in patients undergoing liver resection over a 20-year period[J]. Aliment Pharmacol Ther, 2017, 46(9):856-863. DOI: 10.1111/apt.14261.
|
| [26] |
WONG R J, CHEUNG R, AHMED A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S.[J]. Hepatology, 2014, 59(6):2188-2195. DOI: 10.1002/hep.26986.
|
| [27] |
HONG T P, GOW P, FINK M,et al. Novel population-based study finding higher than reported hepatocellular carcinoma incidence suggests an updated approach is needed[J]. Hepatology, 2016, 63(4):1205-1212. DOI: 10.1002/hep.28267.
|
| [28] |
SEYDA SEYDEL G, KUCUKOGLU O, ALTINBASV A,et al. Economic growth leads to increase of obesity and associated hepatocellular carcinoma in developing countries[J]. Ann Hepatol, 2016, 15(5):662-672. DOI: 10.5604/16652681.1212316.
|
| [29] |
ZHU J Z, ZHOU Q Y, WANG Y M,et al. Prevalence of fatty liver disease and the economy in China:a systematic review[J]. World J Gastroenterol, 2015, 21(18):5695-5706. DOI: 10.3748/wjg.v21.i18.5695.
|
| [30] |
YANG J D, MOHAMED E A, AZIZ A O,et al. Characteristics,management,and outcomes of patients with hepatocellular carcinoma in Africa:a multicountry observational study from the Africa Liver Cancer Consortium[J]. Lancet Gastroenterol Hepatol, 2017, 2(2):103-111. DOI: 10.1016/S2468-1253(16)30161-3.
|
| [31] |
FANZO J C, DOWNS S M. Climate change and nutrition-associated diseases[J]. Nat Rev Dis Primers, 2021, 7(1):90. DOI: 10.1038/s41572-021-00329-3.
|
| [32] |
KOCH C A, SHARDA P, PATEL J,et al. Climate change and obesity[J]. Horm Metab Res, 2021, 53(9):575-587. DOI: 10.1055/a-1533-2861.
|
| [33] |
BLÜHER M. Obesity:global epidemiology and pathogenesis[J]. Nat Rev Endocrinol, 2019, 15(5):288-298. DOI: 10.1038/s41574-019-0176-8.
|
| [34] |
PAFILI K, RODEN M. Nonalcoholic fatty liver disease(NAFLD)from pathogenesis to treatment concepts in humans[J]. Mol Metab, 2021, 50:101122. DOI: 10.1016/j.molmet.2020.101122.
|
| [35] |
SANTORO N, ZHANG C K, ZHAO H Y,et al. Variant in the glucokinase regulatory protein(GCKR)gene is associated with fatty liver in obese children and adolescents[J]. Hepatology, 2012, 55(3):781-789. DOI: 10.1002/hep.24806.
|
| [36] |
STENDER S, KOZLITINA J, NORDESTGAARD B G,et al. Adiposity amplifies the genetic risk of fatty liver disease conferred by multiple loci[J]. Nat Genet, 2017, 49(6):842-847. DOI: 10.1038/ng.3855.
|
| [37] |
KASPER P, MARTIN A, LANG S,et al. NAFLD and cardiovascular diseases:a clinical review[J]. Clin Res Cardiol, 2021, 110(7):921-937. DOI: 10.1007/s00392-020-01709-7.
|
| [38] |
RADU F, POTCOVARU C G, SALMEN T,et al. The link between NAFLD and metabolic syndrome[J]. Diagnostics, 2023, 13(4):614. DOI: 10.3390/diagnostics13040614.
|
| [39] |
KWAK J H, JUN D W, LEE S M,et al. Lifestyle predictors of obese and non-obese patients with nonalcoholic fatty liver disease:a cross-sectional study[J]. Clin Nutr, 2018, 37(5):1550-1557. DOI: 10.1016/j.clnu.2017.08.018.
|
| [40] |
KO E, YOON E L, JUN D W. Risk factors in nonalcoholic fatty liver disease[J]. Clin Mol Hepatol, 2023, 29(Suppl):S79-85. DOI: 10.3350/cmh.2022.0398.
|
| [41] |
ENG J M, ESTALL J L. Diet-induced models of non-alcoholic fatty liver disease:food for thought on sugar,fat,and cholesterol[J]. Cells, 2021, 10(7):1805. DOI: 10.3390/cells10071805.
|
| [42] |
YUAN S, CHEN J, LI X,et al. Lifestyle and metabolic factors for nonalcoholic fatty liver disease:mendelian randomization study[J]. Eur J Epidemiol, 2022, 37(7):723-733. DOI: 10.1007/s10654-022-00868-3.
|
| [43] |
WU F T, PAHKALA K, JUONALA M,et al. Childhood and adulthood passive smoking and nonalcoholic fatty liver in midlife:a 31-year cohort study[J]. Am J Gastroenterol, 2021, 116(6):1256-1263. DOI: 10.14309/ajg.0000000000001141.
|
| [44] |
MUMTAZ H, HAMEED M, SANGAH A B,et al. Association between smoking and non-alcoholic fatty liver disease in Southeast Asia[J]. Front Public Health, 2022, 10:1008878. DOI: 10.3389/fpubh.2022.1008878.
|
| [45] |
JUNG H S, CHANG Y, KWON M J,et al. Smoking and the risk of non-alcoholic fatty liver disease:a cohort study[J]. Am J Gastroenterol, 2019, 114(3):453-463. DOI: 10.1038/s41395-018-0283-5.
|
| [46] |
PREMKUMAR M, ANAND A C. Tobacco,cigarettes,and the liver:the smoking Gun[J]. J Clin Exp Hepatol, 2021, 11(6):700-712. DOI: 10.1016/j.jceh.2021.07.016.
|
| [47] |
HAYAT U, SIDDIQUI A A, OKUT H,et al. The effect of coffee consumption on the non-alcoholic fatty liver disease and liver fibrosis:a meta-analysis of 11 epidemiological studies[J]. Ann Hepatol, 2021, 20:100254. DOI: 10.1016/j.aohep.2020.08.071.
|
| [48] |
ZHANG Y, LIU Z P, CHOUDHURY T,et al. Habitual coffee intake and risk for nonalcoholic fatty liver disease:a two-sample Mendelian randomization study[J]. Eur J Nutr, 2021, 60(4):1761-1767. DOI: 10.1007/s00394-020-02369-z.
|
| [49] |
SANTOS R M M, LIMA D R A. Coffee consumption,obesity and type 2 diabetes:a mini-review[J]. Eur J Nutr, 2016, 55(4):1345-1358. DOI: 10.1007/s00394-016-1206-0.
|
| [50] |
LOOPSTRA-MASTERS R C, LIESE A D, HAFFNER S M,et al. Associations between the intake of caffeinated and decaffeinated coffee and measures of insulin sensitivity and beta cell function[J]. Diabetologia, 2011, 54(2):320-328. DOI: 10.1007/s00125-010-1957-8.
|
| [51] |
SIDORYK K, JAROMIN A, FILIPCZAK N,et al. Synthesis and antioxidant activity of caffeic acid derivatives[J]. Molecules, 2018, 23(9):2199. DOI: 10.3390/molecules23092199.
|
| [52] |
SEO H Y, KIM M K, LEE S H,et al. Kahweol ameliorates the liver inflammation through the inhibition of NF-κB and STAT3 activation in primary kupffer cells and primary hepatocytes[J]. Nutrients, 2018, 10(7):863. DOI: 10.3390/nu10070863.
|
| [53] |
BAJAJ J S, IDILMAN R, MABUDIAN L,et al. Diet affects gut microbiota and modulates hospitalization risk differentially in an international cirrhosis cohort[J]. Hepatology, 2018, 68(1):234-247. DOI: 10.1002/hep.29791.
|
| [54] |
KENNEDY O J, RODERICK P, BUCHANAN R,et al. Coffee,including caffeinated and decaffeinated coffee,and the risk of hepatocellular carcinoma:a systematic review and dose-response meta-analysis[J]. BMJ Open, 2017, 7(5):e013739. DOI: 10.1136/bmjopen-2016-013739.
|
| [55] |
TAMURA T, HISHIDA A, WAKAI. Coffee consumption and liver cancer risk in Japan:a meta-analysis of six prospective cohort studies[J]. Nagoya J Med Sci, 2019, 81(1):143-150. DOI: 10.18999/nagjms.81.1.143.
|
| [56] |
TAMURA T, WADA K, KONISHI K,et al. Coffee,green tea,and caffeine intake and liver cancer risk:a prospective cohort study[J]. Nutr Cancer, 2018, 70(8):1210-1216. DOI: 10.1080/01635581.2018.1512638.
|
| [57] |
VAN DAM R M, HU F B, WILLETT W C. Coffee,caffeine,and health[J]. N Engl J Med, 2020, 383(4):369-378. DOI: 10.1056/NEJMra1816604.
|
| [58] |
WONGTRAKUL W, NILTWAT S, CHARATCHAROENWITTHAYA P. The effects of modest alcohol consumption on non-alcoholic fatty liver disease:a systematic review and meta-analysis[J]. Front Med, 2021, 8:744713. DOI: 10.3389/fmed.2021.744713.
|
| [59] |
AJMERA V, BELT P, WILSON L A,et al. Among patients with nonalcoholic fatty liver disease,modest alcohol use is associated with less improvement in histologic steatosis and steatohepatitis[J]. Clin Gastroenterol Hepatol, 2018, 16(9):1511-1520.e5. DOI: 10.1016/j.cgh.2018.01.026.
|
| [60] |
ROERECKE M, VAFAEI A, HASAN O S M,et al. Alcohol consumption and risk of liver cirrhosis:a systematic review and meta-analysis[J]. Am J Gastroenterol, 2019, 114(10):1574-1586. DOI: 10.14309/ajg.0000000000000340.
|
| [61] |
ÅBERG F, BYRNE C D, PIROLA C J,et al. Alcohol consumption and metabolic syndrome:clinical and epidemiological impact on liver disease[J]. J Hepatol, 2023, 78(1):191-206. DOI: 10.1016/j.jhep.2022.08.030.
|
| [62] |
ALBILLOS A, GOTTARDI A D, RESCIGNO M. The gut-liver axis in liver disease:Pathophysiological basis for therapy[J]. J Hepatol, 2020, 72(3):558-577. DOI: 10.1016/j.jhep.2019.10.003.
|
| [63] |
ZHANG D, HAO X X, XU L L,et al. Intestinal flora imbalance promotes alcohol-induced liver fibrosis by the TGFβ/smad signaling pathway in mice[J]. Oncol Lett, 2017, 14(4):4511-4516. DOI: 10.3892/ol.2017.6762.
|
| [64] |
CHEN Y W, ZHOU J H, WANG L. Role and mechanism of gut microbiota in human disease[J]. Front Cell Infect Microbiol, 2021, 11:625913. DOI: 10.3389/fcimb.2021.625913.
|
| [65] |
WANG D Z, YAN S, YAN J,et al. Effects of triphenyl phosphate exposure during fetal development on obesity and metabolic dysfunctions in adult mice:impaired lipid metabolism and intestinal dysbiosis[J]. Environ Pollut, 2019, 246:630-638. DOI: 10.1016/j.envpol.2018.12.053.
|
| [66] |
ZHU L X, BAKER R D, ZHU R X,et al. Gut microbiota produce alcohol and contribute to NAFLD[J]. Gut, 2016, 65(7):1232. DOI: 10.1136/gutjnl-2016-311571.
|
| [67] |
DE FARIA GHETTI F, OLIVEIRA D G, DE OLIVEIRA J M,et al. Influence of gut microbiota on the development and progression of nonalcoholic steatohepatitis[J]. Eur J Nutr, 2018, 57(3):861-876. DOI: 10.1007/s00394-017-1524-x.
|
| [68] |
FEDERICO A, DALLIO M, GODOS J,et al. Targeting gut-liver axis for the treatment of nonalcoholic steatohepatitis:translational and clinical evidence[J]. Transl Res, 2016, 167(1):116-124. DOI: 10.1016/j.trsl.2015.08.002.
|
| [69] |
LI F X, YE J Z, SHAO C X,et al. Compositional alterations of gut microbiota in nonalcoholic fatty liver disease patients:a systematic review and meta-analysis[J]. Lipids Health Dis, 2021, 20(1):22. DOI: 10.1186/s12944-021-01440-w.
|
| [70] |
OH T G, KIM S M, CAUSSY C,et al. A universal gut-microbiome-derived signature predicts cirrhosis[J]. Cell Metab, 2020, 32(5):901. DOI: 10.1016/j.cmet.2020.10.015.
|
| [71] |
YUAN J, CHEN C, CUI J H,et al. Fatty liver disease caused by high-alcohol-producing Klebsiella pneumoniae[J]. Cell Metab, 2019, 30(6):1172. DOI: 10.1016/j.cmet.2019.11.006.
|
| [72] |
HU H M, LIN A Z, KONG M W,et al. Intestinal microbiome and NAFLD:molecular insights and therapeutic perspectives[J]. J Gastroenterol, 2020, 55(2):142-158. DOI: 10.1007/s00535-019-01649-8.
|
| [73] |
BOURSIER J, MUELLER O, BARRET M,et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota[J]. Hepatology, 2016, 63(3):764-775. DOI: 10.1002/hep.28356.
|
| [74] |
NEWSOME P N, SASSO M, DEEKS J J,et al. FibroScan-AST(FAST)score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis:a prospective derivation and global validation study[J]. Lancet Gastroenterol Hepatol, 2020, 5(4):362-373. DOI: 10.1016/S2468-1253(19)30383-8.
|
| [75] |
FANG J, YU C H, LI X J,et al. Gut dysbiosis in nonalcoholic fatty liver disease:pathogenesis,diagnosis,and therapeutic implications[J]. Front Cell Infect Microbiol, 2022, 12:997018. DOI: 10.3389/fcimb.2022.997018.
|
| [76] |
REN R R, ZHENG Y. Sex differences in cardiovascular and all-cause mortality in nonalcoholic fatty liver disease in the US population[J]. Nutr Metab Cardiovasc Dis, 2023, 33(7):1349-1357. DOI: 10.1016/j.numecd.2023.03.003.
|
| [77] |
DISTEFANO J K. NAFLD and NASH in postmenopausal women:implications for diagnosis and treatment[J]. Endocrinology, 2020, 161(10):bqaa134. DOI: 10.1210/endocr/bqaa134.
|
| [78] |
PALMISANO B T, ZHU L, STAFFORD J M. Role of estrogens in the regulation of liver lipid metabolism[J]. Adv Exp Med Biol, 2017, 1043:227-256. DOI: 10.1007/978-3-319-70178-3_12.
|
| [79] |
JARUVONGVANICH V, SANGUANKEO A, RIANGWIWAT T,et al. Testosterone,sex hormone-binding globulin and nonalcoholic fatty liver disease:a systematic review and meta-analysis[J]. Ann Hepatol, 2017, 16(3):382-394. DOI: 10.5604/16652681.1235481.
|
| [80] |
DONNELLY M C, STABLEFORTH W, KRAG A,et al. The negative bidirectional interaction between climate change and the prevalence and care of liver disease:a joint BSG,BASL,EASL,and AASLD commentary[J]. J Hepatol, 2022, 76(5):995-1000. DOI: 10.1016/j.jhep.2022.02.012.
|
| [81] |
LI W, XIAO H T, WU H,et al. Analysis of environmental chemical mixtures and nonalcoholic fatty liver disease:NHANES 1999-2014[J]. Environ Pollut, 2022, 311:119915. DOI: 10.1016/j.envpol.2022.119915.
|
| [82] |
|
| [83] |
HADLEY K, WHEAT S, ROGERS H H,et al. Mechanisms underlying food insecurity in the aftermath of climate-related shocks:a systematic review[J]. Lancet Planet Health, 2023, 7(3):e242-250. DOI: 10.1016/S2542-5196(23)00003-7.
|
| [84] |
CANO R, PÉREZ J L, DÁVILA L A,et al. Role of endocrine-disrupting chemicals in the pathogenesis of non-alcoholic fatty liver disease:a comprehensive review[J]. Int J Mol Sci, 2021, 22(9):4807. DOI: 10.3390/ijms22094807.
|
| [85] |
ZHANG X Y, ZHAO L G, DUCATMAN A,et al. Association of per- and polyfluoroalkyl substance exposure with fatty liver disease risk in US adults[J]. JHEP Rep, 2023, 5(5):100694. DOI: 10.1016/j.jhepr.2023.100694.
|
| [86] |
AN S J, YANG E J, OH S,et al. The association between urinary bisphenol A levels and nonalcoholic fatty liver disease in Korean adults:Korean National Environmental Health Survey(KoNEHS)2015-2017[J]. Environ Health Prev Med, 2021, 26(1):91. DOI: 10.1186/s12199-021-01010-7.
|
| [87] |
FLING R R, ZACHAREWSKI T R. Aryl hydrocarbon receptor(AhR)activation by 2,3,7,8-tetrachlorodibenzo- p-dioxin(TCDD)dose-dependently shifts the gut microbiome consistent with the progression of non-alcoholic fatty liver disease[J]. Int J Mol Sci, 2021, 22(22):12431. DOI: 10.3390/ijms222212431.
|
| [88] |
ZHU X Y, XIA H G, WANG Z H,et al. In vitro and in vivo approaches for identifying the role of aryl hydrocarbon receptor in the development of nonalcoholic fatty liver disease[J]. Toxicol Lett, 2020, 319:85-94. DOI: 10.1016/j.toxlet.2019.10.010.
|
| [89] |
KIM K, MELOUGH M M, VANCE T M,et al. Dietary cadmium intake and sources in the US[J]. Nutrients, 2018, 11(1):2. DOI: 10.3390/nu11010002.
|
| [90] |
LI Y X, CHEN C, LU L P,et al. Cadmium exposure in young adulthood is associated with risk of nonalcoholic fatty liver disease in midlife[J]. Dig Dis Sci, 2022, 67(2):689-696. DOI: 10.1007/s10620-021-06869-8.
|
| [91] |
PARK E, KIM J, KIM B,et al. Association between environmental exposure to cadmium and risk of suspected non-alcoholic fatty liver disease[J]. Chemosphere, 2021, 266:128947. DOI: 10.1016/j.chemosphere.2020.128947.
|
| [92] |
CAVE M, APPANA S, PATEL M,et al. Polychlorinated biphenyls,lead,and mercury are associated with liver disease in American adults:NHANES 2003-2004[J]. Environ Health Perspect, 2010, 118(12):1735-1742. DOI: 10.1289/ehp.1002720.
|
| [93] |
FREDIANI J K, NAIOTI E A, VOS M B,et al. Arsenic exposure and risk of nonalcoholic fatty liver disease(NAFLD)among U.S. adolescents and adults:an association modified by race/ethnicity,NHANES 2005-2014[J]. Environ Health, 2018, 17(1):6. DOI: 10.1186/s12940-017-0350-1.
|
| [94] |
YANG C Y, LI Y Y, DING R,et al. Lead exposure as a causative factor for metabolic associated fatty liver disease(MAFLD)and a lead exposure related nomogram for MAFLD prevalence[J]. Front Public Health, 2022, 10:1000403. DOI: 10.3389/fpubh.2022.1000403.
|
| [95] |
YOUNG J L, CAVE M C, XU Q,et al. Whole life exposure to low dose cadmium alters diet-induced NAFLD[J]. Toxicol Appl Pharmacol, 2022, 436:115855. DOI: 10.1016/j.taap.2021.115855.
|
| [96] |
GU J, KONG A Q, GUO C Z,et al. Cadmium perturbed lipid profile and induced liver dysfunction in mice through phosphatidylcholine remodeling and promoting arachidonic acid synthesis and metabolism[J]. Ecotoxicol Environ Saf, 2022, 247:114254. DOI: 10.1016/j.ecoenv.2022.114254.
|
| [97] |
QIU T M, PEI P, YAO X F,et al. Taurine attenuates arsenic-induced pyroptosis and nonalcoholic steatohepatitis by inhibiting the autophagic-inflammasomal pathway[J]. Cell Death Dis, 2018, 9(10):946. DOI: 10.1038/s41419-018-1004-0.
|
| [98] |
CHEN H G, ZHU C X, ZHOU X. Effects of lead and cadmium combined heavy metals on liver function and lipid metabolism in mice[J]. Biol Trace Elem Res, 2023, 201(6):2864-2876. DOI: 10.1007/s12011-022-03390-5.
|
| [99] |
AUGUET T, BERTRAN L, BARRIENTOS-RIOSALIDO A,et al. Are ingested or inhaled microplastics involved in nonalcoholic fatty liver disease?[J]. Int J Environ Res Public Health, 2022, 19(20):13495. DOI: 10.3390/ijerph192013495.
|
| [100] |
LI L, XU M J, HE C,et al. Polystyrene nanoplastics potentiate the development of hepatic fibrosis in high fat diet fed mice[J]. Environ Toxicol, 2022, 37(2):362-372. DOI: 10.1002/tox.23404.
|
| [101] |
YIN J L, JU Y, QIAN H H,et al. Nanoplastics and microplastics may be damaging our livers[J]. Toxics, 2022, 10(10):586. DOI: 10.3390/toxics10100586.
|
| [102] |
YEE M S, HII L W, LOOI C K,et al. Impact of microplastics and nanoplastics on human health[J]. Nanomaterials, 2021, 11(2):496. DOI: 10.3390/nano11020496.
|
| [103] |
CHENG W, LI X L, ZHOU Y,et al. Polystyrene microplastics induce hepatotoxicity and disrupt lipid metabolism in the liver organoids[J]. Sci Total Environ, 2022, 806(Pt 1):150328. DOI: 10.1016/j.scitotenv.2021.150328.
|
| [104] |
LAI W C, XU D, LI J M,et al. Dietary polystyrene nanoplastics exposure alters liver lipid metabolism and muscle nutritional quality in carnivorous marine fish large yellow croaker(Larimichthys crocea)[J]. J Hazard Mater, 2021, 419:126454. DOI: 10.1016/j.jhazmat.2021.126454.
|
| [105] |
THANGAVEL P, PARK D, LEE Y C. Recent insights into particulate matter(PM2.5)-mediated toxicity in humans:an overview[J]. Int J Environ Res Public Health, 2022, 19(12):7511. DOI: 10.3390/ijerph19127511.
|
| [106] |
SUN S Z, YANG Q Q, ZHOU Q X,et al. Long-term exposure to fine particulate matter and non-alcoholic fatty liver disease:a prospective cohort study[J]. Gut, 2022, 71(2):443-445. DOI: 10.1136/gutjnl-2021-324364.
|
| [107] |
XU J X, ZHANG W, LU Z B,et al. Airborne PM2.5-induced hepatic insulin resistance by Nrf2/JNK-mediated signaling pathway[J]. Int J Environ Res Public Health, 2017, 14(7):787. DOI: 10.3390/ijerph14070787.
|
| [108] |
XU Z J, SHI L M, LI D C,et al. Real ambient particulate matter-induced lipid metabolism disorder:roles of peroxisome proliferators-activated receptor alpha[J]. Ecotoxicol Environ Saf, 2022, 231:113173. DOI: 10.1016/j.ecoenv.2022.113173.
|
| [109] |
XU X H, LIU C Q, XU Z B,et al. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue[J]. Toxicol Sci, 2011, 124(1):88-98. DOI: 10.1093/toxsci/kfr211.
|
| [110] |
FERRO D, BARATTA F, PASTORI D,et al. New insights into the pathogenesis of non-alcoholic fatty liver disease:gut-derived lipopolysaccharides and oxidative stress[J]. Nutrients, 2020, 12(9):2762. DOI: 10.3390/nu12092762.
|
| [111] |
LONG M H, ZHANG C, XU D Q,et al. PM2.5 aggravates diabetes via the systemically activated IL-6-mediated STAT3/SOCS3 pathway in rats' liver[J]. Environ Pollut, 2020, 256:113342. DOI: 10.1016/j.envpol.2019.113342.
|
| [112] |
LI R, SUN Q, LAM S M,et al. Sex-dependent effects of ambient PM2.5 pollution on insulin sensitivity and hepatic lipid metabolism in mice[J]. Part Fibre Toxicol, 2020, 17(1):14. DOI: 10.1186/s12989-020-00343-5.
|
 )
)