中国全科医学 ›› 2023, Vol. 26 ›› Issue (35): 4425-4432.DOI: 10.12114/j.issn.1007-9572.2023.0260
刘林波1, 廖智杰1, 杨文凡2, 白丹丹1, 王冬梅1, 施森2,*( )
)
收稿日期:2023-03-28
修回日期:2023-07-06
出版日期:2023-12-15
发布日期:2023-07-27
通讯作者:
施森
基金资助:
LIU Linbo1, LIAO Zhijie1, YANG Wenfan2, BAI Dandan1, WANG Dongmei1, SHI Sen2,*( )
)
Received:2023-03-28
Revised:2023-07-06
Published:2023-12-15
Online:2023-07-27
Contact:
SHI Sen
摘要: 背景 周围动脉疾病(PAD)是心血管疾病中一种常见的、严重的疾病,易并发肢体缺血及心血管不良事件。PAD的患病有性别差异,而相关研究相对缺乏。充分认识中国PAD患病情况的性别差异对于公共卫生政策的制定至关重要。 目的 分析中国PAD患病情况中的性别差异及其原因,为制订有针对性的筛查和预防措施提供理论依据。 方法 通过2019年全球疾病负担(GBD)数据库提取中国男性和女性以及全球、日本、韩国和印度女性的PAD患病人数、患病率、年龄标化患病率、疾病负担可归因危险因素以及相应95%不确定区间(UI)。采用R语言进行本研究数据和可视化分析。采用Joinpoint软件分析1990—2019年中国男性和女性PAD患病率随时间变化的趋势,计算PAD患病率的年度变化百分比(APC)和平均年度变化百分比(AAPC)以及其95%可信区间(CI)。采用贝叶斯年龄-时期-队列(BAPC)模型预测2020—2035年PAD的患病人数和患病率。 结果 中国2019年PAD患病率例数男性为71.74×10万,女性为213.15×10万。与1990年比较,2019年PAD患病人数男性增加了154.22%,女性增加了181.27%。2019年日本、韩国、印度和全球女性PAD患病人数、患病率均较1990年升高,但年龄标化患病率均降低,1990年中国女性PAD年龄标化患病率分别为日本和韩国女性的57.80%和76.35%,2019年则分别为日本和韩国的1.10倍和1.33倍。中国男性PAD患病率1990年为462.40/10万,2019年为989.79/10万,增幅为114.05%,1990—2019年呈上升趋势。中国女性PAD的患病率1990年为1 321.44/10万,2019年为3 055.85/10万,增幅为131.25%,1990—2019年呈上升趋势。2019年中国女性PAD患病率是男性的3.09倍。中国男性PAD的年龄标化患病率1990年为731.02/10万,2019年为744.96/10万,增幅为1.91%,1990—1993年、1993—2005年呈上升趋势,2005—2019年呈下降趋势。中国女性PAD的年龄标化患病率1990年为1 839.43/10万,2019年为2 022.13/10万,增幅为9.93%,1990—2005年呈上升趋势(P<0.05),2005—2019年变化趋势不显著(P>0.05)。2019年中国女性PAD年龄标化患病率是男性的2.71倍。BAPC模型预测结果示,2035年中国男性PAD患病人数将达到101.30×10万,女性将达到319.24×10万。2035年中国女性PAD患病人数较2019年将增长49.77%。分年龄统计,2019年中国女性65~69岁PAD患病人数最多,为35.15×10万,2035年将是70~74岁患病人数最多,为55.89×10万。2035年40~44、45~49、50~54、55~59岁中国女性PAD患病人数将低于2019年,60~64、65~69、70~74、75~79、80~84、85~89、90~94、≥95岁患病人数将高于2019年。2035年中国男性PAD年龄标化患病率为712.09/10万,女性为1 945.97/10万,较2019年分别降低4.41%与3.77%。分年龄统计,2035年中国女性各年龄分层PAD患病率随年龄增大而增加,除≥95岁人群外,其他年龄段人群的患病率均较2019年下降。2019年中国PAD疾病负担可归因于6种危险因素,分别为高血压、吸烟、糖尿病、肾功能不全、高盐饮食和铅暴露。男性最主要危险因素为吸烟(44.32%),其次为高血压(18.97%)和糖尿病(16.11%)。女性最主要的危险因素为高血压(32.31%),其次为糖尿病(24.81%)和肾功能不全(17.27%)。 结论 中国女性PAD的患病人数、患病率及年龄标化患病率均明显高于男性,并且年龄标化患病率已经超过日本和韩国。在可预知的未来,中国女性PAD患病人数将进一步增加,且老年女性的患病人数增长越来越明显。因此应更加重视PAD在性别、年龄方面呈现出的变化,重视PAD患者危险因素的性别差异,采取必要的筛查和预防措施。
| 地区 | 性别 | 患病人数 | 粗患病率 | 年龄标化患病率 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990年(95%UI)(×10万) | 2019年(95%UI)(×10万) | 变化率(%) | 1990年(95%UI)(1/10万) | 2019年(95%UI)(1/10万) | 变化率(%) | 1990年(95%UI)(1/10万) | 2019年(95%UI)(1/10万) | 变化率(%) | ||
| 中国 | 男性 | 28.22(24.03,32.53) | 71.74(61.29,82.49) | 154.22 | 462.40(393.73,533.09) | 989.79(845.60,1 138.07) | 114.05 | 731.02(631.44,836.51) | 744.96(644.62,850.82) | 1.91 |
| 女性 | 75.78(65.04,86.78) | 213.15(183.34,244.52) | 181.27 | 1 321.44(1 134.16,1 513.18) | 3 055.85(2 628.40,3 505.48) | 131.25 | 1 839.43(1 593.06,2 095.46) | 2 022.13(1 750.00,2 309.13) | 9.93 | |
| 日本 | 女性 | 30.72(26.73,34.70) | 37.26(32.11,42.65) | 21.29 | 4 801.14(4 177.38,5 422.56) | 5 686.97(4 901.04,6 509.51) | 18.45 | 3 182.64(2 782.59,3 587.70) | 1 846.52(1 606.47,2 091.10) | -41.98 |
| 韩国 | 女性 | 3.88(3.34,4.42) | 7.53(6.51,8.61) | 94.07 | 1 756.55(1 512.74,2 001.33) | 2 850.98(2 466.53,3 260.43) | 62.31 | 2 409.29(2 083.25,2 739.95) | 1 519.64(1 314.65,1 737.66) | -36.93 |
| 印度 | 女性 | 21.43(18.33,24.63) | 61.15(52.96,70.11) | 185.35 | 522.29(446.86,600.39) | 902.56(781.69,1 034.75) | 72.81 | 1 135.33(985.40,1 300.95) | 1 105.89(959.02,1 261.32) | -2.59 |
| 全球 | 女性 | 447.95(390.62,507.73) | 760.93(665.87,861.71) | 69.87 | 1 686.50(1 470.66,1 911.55) | 1 973.12(1 726.63,2 234.45) | 16.99 | 2 181.02(1 905.72,2 471.79) | 1 735.06(1 519.05,1 964.04) | -20.45 |
表1 1990年和2019年中国男性和中国、日本、韩国、印度及全球女性PAD患病情况
Table 1 Prevalence of PAD among Chinese men and women in China,Japan,Korea,India and globally in 1990 and 2019
| 地区 | 性别 | 患病人数 | 粗患病率 | 年龄标化患病率 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1990年(95%UI)(×10万) | 2019年(95%UI)(×10万) | 变化率(%) | 1990年(95%UI)(1/10万) | 2019年(95%UI)(1/10万) | 变化率(%) | 1990年(95%UI)(1/10万) | 2019年(95%UI)(1/10万) | 变化率(%) | ||
| 中国 | 男性 | 28.22(24.03,32.53) | 71.74(61.29,82.49) | 154.22 | 462.40(393.73,533.09) | 989.79(845.60,1 138.07) | 114.05 | 731.02(631.44,836.51) | 744.96(644.62,850.82) | 1.91 |
| 女性 | 75.78(65.04,86.78) | 213.15(183.34,244.52) | 181.27 | 1 321.44(1 134.16,1 513.18) | 3 055.85(2 628.40,3 505.48) | 131.25 | 1 839.43(1 593.06,2 095.46) | 2 022.13(1 750.00,2 309.13) | 9.93 | |
| 日本 | 女性 | 30.72(26.73,34.70) | 37.26(32.11,42.65) | 21.29 | 4 801.14(4 177.38,5 422.56) | 5 686.97(4 901.04,6 509.51) | 18.45 | 3 182.64(2 782.59,3 587.70) | 1 846.52(1 606.47,2 091.10) | -41.98 |
| 韩国 | 女性 | 3.88(3.34,4.42) | 7.53(6.51,8.61) | 94.07 | 1 756.55(1 512.74,2 001.33) | 2 850.98(2 466.53,3 260.43) | 62.31 | 2 409.29(2 083.25,2 739.95) | 1 519.64(1 314.65,1 737.66) | -36.93 |
| 印度 | 女性 | 21.43(18.33,24.63) | 61.15(52.96,70.11) | 185.35 | 522.29(446.86,600.39) | 902.56(781.69,1 034.75) | 72.81 | 1 135.33(985.40,1 300.95) | 1 105.89(959.02,1 261.32) | -2.59 |
| 全球 | 女性 | 447.95(390.62,507.73) | 760.93(665.87,861.71) | 69.87 | 1 686.50(1 470.66,1 911.55) | 1 973.12(1 726.63,2 234.45) | 16.99 | 2 181.02(1 905.72,2 471.79) | 1 735.06(1 519.05,1 964.04) | -20.45 |
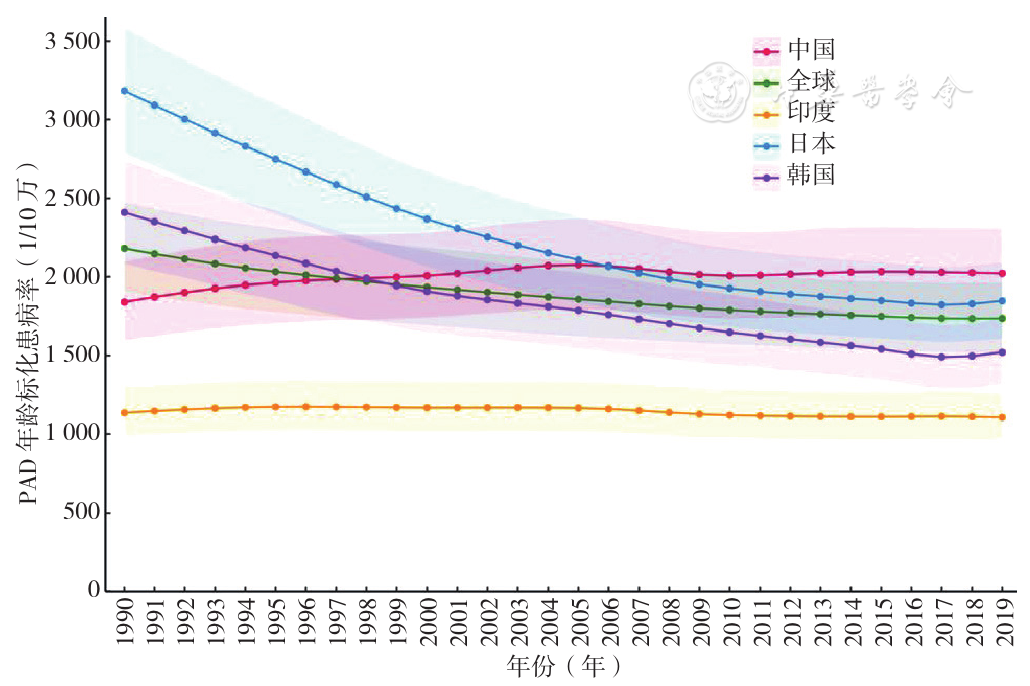
图1 1990—2019年全球、中国、印度、日本、韩国女性PAD年龄标化患病率变化趋势注:PAD=周围动脉疾病。
Figure 1 Trends in the age-standardized prevalence of PAD in women from 1990 to 2019 in globally,China,India,Japan,and Korea
| 项目 | 性别 | 趋势1 | 趋势2 | 趋势3 | AAPC(95%CI) | |||
|---|---|---|---|---|---|---|---|---|
| 年份 | APC(95%CI) | 年份 | APC(95%CI) | 年份 | APC(95%CI) | |||
| 粗患病率 | 男性 | 1990—1999年 | 2.58(2.52,2.65)a | 1999—2007年 | 3.17(3.07,3.26)a | 2007—2019年 | 2.39(2.34,2.43)a | 2.66(2.63,2.70)a |
| 女性 | 1990—2006年 | 2.90(2.84,2.96)a | 2006—2009年 | 2.21(0.67,3.77)a | 2009—2019年 | 3.24(3.11,3.36)a | 2.94(2.78,3.10)a | |
| 年龄标化患病率 | 男性 | 1990—1993年 | 0.91(0.68,1.14)a | 1993—2005年 | 0.49(0.46,0.52)a | 2005—2019年 | -0.50(-0.52,-0.48)a | 0.05(0.03,0.08)a |
| 女性 | 1990—2005年 | 0.73(0.65,0.81)a | 2005—2009年 | -0.93(-1.87,0.03) | 2009—2019年 | 0.10(-0.05,0.25) | 0.28(0.14,0.42)a | |
表2 1990—2019年中国PAD粗患病率和年龄标化患病率时间变化趋势
Table 2 Temporal changes of PAD prevalence and age-standardized prevalence in China from 1990 to 2019
| 项目 | 性别 | 趋势1 | 趋势2 | 趋势3 | AAPC(95%CI) | |||
|---|---|---|---|---|---|---|---|---|
| 年份 | APC(95%CI) | 年份 | APC(95%CI) | 年份 | APC(95%CI) | |||
| 粗患病率 | 男性 | 1990—1999年 | 2.58(2.52,2.65)a | 1999—2007年 | 3.17(3.07,3.26)a | 2007—2019年 | 2.39(2.34,2.43)a | 2.66(2.63,2.70)a |
| 女性 | 1990—2006年 | 2.90(2.84,2.96)a | 2006—2009年 | 2.21(0.67,3.77)a | 2009—2019年 | 3.24(3.11,3.36)a | 2.94(2.78,3.10)a | |
| 年龄标化患病率 | 男性 | 1990—1993年 | 0.91(0.68,1.14)a | 1993—2005年 | 0.49(0.46,0.52)a | 2005—2019年 | -0.50(-0.52,-0.48)a | 0.05(0.03,0.08)a |
| 女性 | 1990—2005年 | 0.73(0.65,0.81)a | 2005—2009年 | -0.93(-1.87,0.03) | 2009—2019年 | 0.10(-0.05,0.25) | 0.28(0.14,0.42)a | |
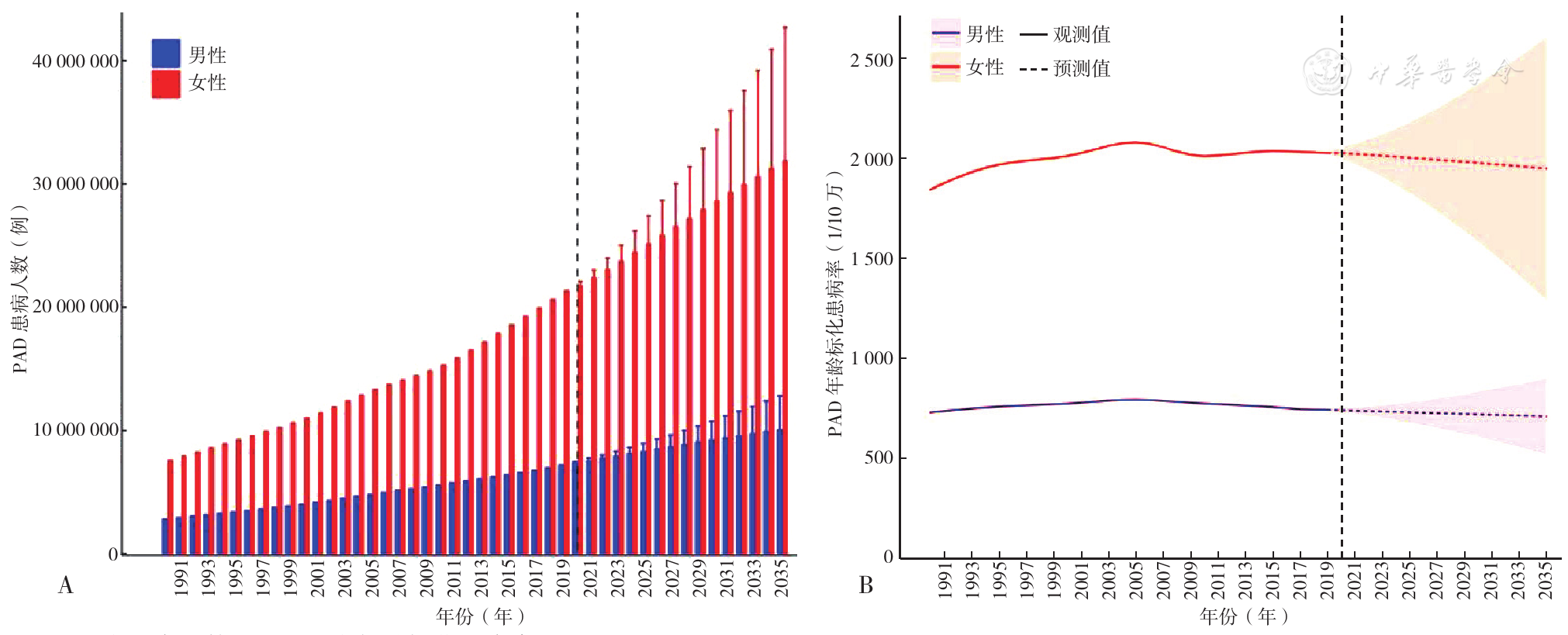
图4 2020—2035年中国PAD性别患病人数和年龄标化患病率变化趋势预测注:A为患病人数预测,B为年龄标化患病率预测。
Figure 4 Prediction of the changing trend of the number cases and age-standardized prevalence of PAD by gender in China from 2020 to 2035
| 分层 | 患病人数 | 年龄标化患病率/年龄分层患病率 | ||||
|---|---|---|---|---|---|---|
| 2019年(×10万) | 2035年(×10万) | 变化率(%) | 2019年(1/10万) | 2035年(1/10万) | 变化率(%) | |
| 男性 | 71.74(61.29,82.49) | 101.30(74.17,128.43) | 41.20 | 744.96(644.62,850.82) | 712.09(521.26,902.92) | -4.41 |
| 女性 | 213.15(183.34,244.52) | 319.24(211.74,426.74) | 49.77 | 2 022.13(1 750.00,2 309.13) | 1 945.97(1 290.41,2 601.54) | -3.77 |
| 年龄 | ||||||
| 40~44岁 | 3.53(2.63,4.53) | 3.44(2.03,4.86) | -2.55 | 709.33(528.11,909.28) | 685.46(451.91,997.17) | -3.37 |
| 45~49岁 | 10.28(8.00,13.02) | 10.23(6.48,13.98) | -0.49 | 1 727.05(1 343.83,2 186.38) | 1 669.34(1 141.36,2 356.88) | -3.34 |
| 50~54岁 | 20.45(15.47,26.47) | 16.84(10.99,22.68) | -17.65 | 3 283.85(2 484.01,4 250.95) | 3 176.14(2 211.35,4 416.94) | -3.28 |
| 55~59岁 | 24.22(18.92,29.50) | 23.60(15.55,31.65) | -2.56 | 5 130.90(4 009.67,6 250.79) | 4 954.32(3 467.83,6 858.72) | -3.44 |
| 60~64岁 | 28.05(21.86,34.20) | 37.79(24.90,50.67) | 34.72 | 7 174.76(5 591.51,8 748.45) | 6 911.64(4 838.26,9 567.32) | -3.67 |
| 65~69岁 | 35.15(28.53,42.76) | 54.23(35.74,72.71) | 54.28 | 9 808.05(7 962.41,11 931.32) | 9 534.03(6 674.27,13 197.34) | -2.79 |
| 70~74岁 | 31.48(24.75,38.93) | 55.89(36.84,74.94) | 77.54 | 12 834.99(10 090.64,15 872.26) | 12 644.82(8 851.97,17 502.76) | -1.48 |
| 75~79岁 | 24.68(19.95,29.94) | 47.23(31.13,63.32) | 91.37 | 15 710.38(12 701.39,19 056.28) | 15 578.80(10 906.09,21 564.03) | -0.84 |
| 80~84岁 | 19.50(15.94,23.57) | 42.34(27.91,56.77) | 117.10 | 18 233.42(14 904.87,22 040.04) | 18 047.91(12 634.59,24 981.53) | -1.02 |
| 85~89岁 | 11.03(9.15,13.23) | 22.05(14.54,29.57) | 99.91 | 19 956.90(16 549.96,23 939.22) | 19 644.12(13 752.07,27 191.05) | -1.57 |
| 90~94岁 | 3.90(3.26,4.62) | 8.00(5.28,10.73) | 105.10 | 21 005.15(17 575.78,24 849.58) | 20 503.84(14 353.82,28 381.23) | -2.39 |
| ≥95岁 | 0.89(0.74,1.06) | 2.42(1.59,3.24) | 171.90 | 19 900.02(16 381.60,23 738.57) | 21 118.14(14 783.68,29 231.74) | 6.12 |
表3 2019年和2035年中国PAD患病人数和年龄标化患病率比较
Table 3 Comparison of number of cases and age-standardized prevalence of PAD in China in 2019 and 2035
| 分层 | 患病人数 | 年龄标化患病率/年龄分层患病率 | ||||
|---|---|---|---|---|---|---|
| 2019年(×10万) | 2035年(×10万) | 变化率(%) | 2019年(1/10万) | 2035年(1/10万) | 变化率(%) | |
| 男性 | 71.74(61.29,82.49) | 101.30(74.17,128.43) | 41.20 | 744.96(644.62,850.82) | 712.09(521.26,902.92) | -4.41 |
| 女性 | 213.15(183.34,244.52) | 319.24(211.74,426.74) | 49.77 | 2 022.13(1 750.00,2 309.13) | 1 945.97(1 290.41,2 601.54) | -3.77 |
| 年龄 | ||||||
| 40~44岁 | 3.53(2.63,4.53) | 3.44(2.03,4.86) | -2.55 | 709.33(528.11,909.28) | 685.46(451.91,997.17) | -3.37 |
| 45~49岁 | 10.28(8.00,13.02) | 10.23(6.48,13.98) | -0.49 | 1 727.05(1 343.83,2 186.38) | 1 669.34(1 141.36,2 356.88) | -3.34 |
| 50~54岁 | 20.45(15.47,26.47) | 16.84(10.99,22.68) | -17.65 | 3 283.85(2 484.01,4 250.95) | 3 176.14(2 211.35,4 416.94) | -3.28 |
| 55~59岁 | 24.22(18.92,29.50) | 23.60(15.55,31.65) | -2.56 | 5 130.90(4 009.67,6 250.79) | 4 954.32(3 467.83,6 858.72) | -3.44 |
| 60~64岁 | 28.05(21.86,34.20) | 37.79(24.90,50.67) | 34.72 | 7 174.76(5 591.51,8 748.45) | 6 911.64(4 838.26,9 567.32) | -3.67 |
| 65~69岁 | 35.15(28.53,42.76) | 54.23(35.74,72.71) | 54.28 | 9 808.05(7 962.41,11 931.32) | 9 534.03(6 674.27,13 197.34) | -2.79 |
| 70~74岁 | 31.48(24.75,38.93) | 55.89(36.84,74.94) | 77.54 | 12 834.99(10 090.64,15 872.26) | 12 644.82(8 851.97,17 502.76) | -1.48 |
| 75~79岁 | 24.68(19.95,29.94) | 47.23(31.13,63.32) | 91.37 | 15 710.38(12 701.39,19 056.28) | 15 578.80(10 906.09,21 564.03) | -0.84 |
| 80~84岁 | 19.50(15.94,23.57) | 42.34(27.91,56.77) | 117.10 | 18 233.42(14 904.87,22 040.04) | 18 047.91(12 634.59,24 981.53) | -1.02 |
| 85~89岁 | 11.03(9.15,13.23) | 22.05(14.54,29.57) | 99.91 | 19 956.90(16 549.96,23 939.22) | 19 644.12(13 752.07,27 191.05) | -1.57 |
| 90~94岁 | 3.90(3.26,4.62) | 8.00(5.28,10.73) | 105.10 | 21 005.15(17 575.78,24 849.58) | 20 503.84(14 353.82,28 381.23) | -2.39 |
| ≥95岁 | 0.89(0.74,1.06) | 2.42(1.59,3.24) | 171.90 | 19 900.02(16 381.60,23 738.57) | 21 118.14(14 783.68,29 231.74) | 6.12 |
| 危险因素 | 女性 | 男性 |
|---|---|---|
| 高血压 | 32.31 | 18.97 |
| 糖尿病 | 24.81 | 16.11 |
| 肾功能不全 | 17.27 | 10.66 |
| 吸烟 | 14.91 | 44.32 |
| 高盐饮食 | 8.40 | 7.81 |
| 铅暴露 | 2.30 | 2.13 |
表4 2019年中国PAD疾病负担危险因素占比(%)
Table 4 Proportion of risk factors of PAD disease burden in China in 2019
| 危险因素 | 女性 | 男性 |
|---|---|---|
| 高血压 | 32.31 | 18.97 |
| 糖尿病 | 24.81 | 16.11 |
| 肾功能不全 | 17.27 | 10.66 |
| 吸烟 | 14.91 | 44.32 |
| 高盐饮食 | 8.40 | 7.81 |
| 铅暴露 | 2.30 | 2.13 |
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
李辉章,杜灵彬. Joinpoint回归模型在肿瘤流行病学时间趋势分析中的应用[J]. 中华预防医学杂志,2020,54(8):908-912. DOI:10.3760/cma.j.cn112150-20200616-00889.
|
| [17] |
王红心,樊文龙,杨晓雨,等. 1990—2019年中国蛋白质能量营养不良发病趋势及预测研究[J]. 中国全科医学,2023,26(5):591-597. DOI:10.12114/j.issn.1007-9572.2022.0556.
|
| [18] |
许晴晴,严永富,陈浩,等. 中国四大慢性病死亡率可持续发展目标实现的预测研究[J]. 中华流行病学杂志,2022,43(6):878-884. DOI:10.3760/cma.j.cn112338-20211028-00830.
|
| [19] |
梁珊珊,周智华,李成程,等. 1990—2019年中国糖尿病疾病负担及发病预测分析[J]. 中国全科医学,2023,26(16):2013-2019. DOI:10.12114/j.issn.1007-9572.2023.0009.
|
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
项鑫,王乙. 中国人口老龄化现状、特点、原因及对策[J]. 中国老年学杂志,2021,41(18):4149-4152. DOI:10.3969/j.issn.1005-9202.2021.18.072.
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [34] |
|
| [35] |
|
| [36] |
|
| [37] |
|
| [38] |
|
| [39] |
|
| [40] |
|
| [41] |
赵倩南,王淳秀,关绍晨,等. 北京地区35岁及以上人群外周动脉疾病患病率特点及影响因素分析[J]. 中华心血管病杂志,2019,47(12):1000-1004. DOI:10.3760/cma.j.issn.0253?3758.2019.12.010.
|
| [42] |
蔡毅,崔华,范利. 北京市军队老年男性高血压患者心脑血管疾病患病率调查[J]. 中国康复理论与实践,2015,21(11):1298-1303. DOI:10.3969/j.issn.1006-9771.2015.11.014.
|
| [43] |
李宪凯,韩扬,徐大春,等. 踝臂指数与外周动脉疾病死亡率之间的关系[J]. 同济大学学报(医学版),2015,36(2):74-80. DOI:10.16118/j.1008-0392.2015.02.017.
|
| [44] |
|
| [45] |
|
| [46] |
|
| [47] |
|
| [48] |
|
| [49] |
|
| [50] |
|
| [1] | 王丽娜, 高鹏飞, 曹帆, 葛莹, 颜维, 何岱昆. 不同性别人群非酒精性脂肪性肝病患病现况及影响因素分析[J]. 中国全科医学, 2023, 26(33): 4143-4151. |
| [2] | 蹇秋枫, 徐荣华, 姚倩, 周媛媛. 中国老年脑卒中患者认知障碍患病率和影响因素的Meta分析[J]. 中国全科医学, 2023, 26(32): 4070-4079. |
| [3] | 马丽媛, 王增武, 樊静, 胡盛寿. 《中国心血管健康与疾病报告2022》要点解读[J]. 中国全科医学, 2023, 26(32): 3975-3994. |
| [4] | 何莉, 张逸凡, 沈雪纯, 孙燕, 赵洋. 中国大陆地区居民慢性病共病的流行趋势:一项Meta分析[J]. 中国全科医学, 2023, 26(29): 3599-3607. |
| [5] | 田美玲, 马国娟, 杜立燕, 肖远革, 张赛, 张翠, 唐增军. 2014—2021年河北省妊娠期糖尿病患病率及流行病学研究[J]. 中国全科医学, 2023, 26(26): 3320-3324. |
| [6] | 杨璐, 宗占红, 易莹莹. 中国农村中老年女性抑郁状况及影响因素研究[J]. 中国全科医学, 2023, 26(25): 3091-3095. |
| [7] | 林洋, 王芳, 王寒, 武蓉, 王瑶, 徐子尧, 王旭, 王彦丁. 老年共病患者衰弱患病率的Meta分析[J]. 中国全科医学, 2023, 26(25): 3185-3193. |
| [8] | 孙旭海, 石秀秀, 赵峥峥, 韩金祥. 2011—2021年北京市某社区新增与死亡严重精神障碍患者特征分析[J]. 中国全科医学, 2023, 26(19): 2402-2407. |
| [9] | 葛安心, 张桂青, 蒋良, 邢文龙, 胡敏, 李浩浩, 孟瑶. 新疆维吾尔自治区精神障碍流行病学调查及影响因素研究[J]. 中国全科医学, 2023, 26(19): 2395-2401. |
| [10] | 贺嘉慧, 李培雯, 马喜民, 乔慧. 西部地区农村居民两周患病未就诊影响因素研究[J]. 中国全科医学, 2023, 26(16): 1946-1952. |
| [11] | 刘雅鑫, 蒋运兰, 黄孝星, 潘竟, 沈音丽, 张越. 中国老年人吞咽障碍患病率的Meta分析[J]. 中国全科医学, 2023, 26(12): 1496-1502. |
| [12] | 段朝晖, 张敏, 徐杰茹, 熊文婧, 陈磊, 赵湘铃, 张译匀, 让蔚清. 2000—2019年中国脑瘤死亡趋势分析及预测研究[J]. 中国全科医学, 2023, 26(06): 734-741. |
| [13] | 王红心, 樊文龙, 杨晓雨, 陈东宇, 黄巧, 潘素跃, 王朴, 胡敏, 何玉清. 1990—2019年中国蛋白质能量营养不良发病趋势及预测研究[J]. 中国全科医学, 2023, 26(05): 591-597. |
| [14] | 刘凤东, 张博强, 阎涵, 井丽, 于晓晨, 王丽, 刘云飞, 邢立莹, 田园梦. 缺血性脑卒中患者糖尿病患病现状及影响因素研究[J]. 中国全科医学, 2023, 26(02): 175-183. |
| [15] | 齐元涛, 柳言, 杜金, 刘永文, 马桂峰. 基于健康生态学模型的我国老年人慢性病共病影响因素研究[J]. 中国全科医学, 2023, 26(01): 50-57. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





