中国全科医学 ›› 2023, Vol. 26 ›› Issue (20): 2459-2468.DOI: 10.12114/j.issn.1007-9572.2023.0068
费敏1, 雷思1, 许琰1, 叶云1, 卓慧1, 张慧2,*( ), 罗荧荃1,*(
), 罗荧荃1,*( )
)
收稿日期:2022-12-04
修回日期:2023-03-03
出版日期:2023-07-15
发布日期:2023-03-21
通讯作者:
张慧, 罗荧荃
基金资助:
FEI Min1, LEI Si1, XU Yan1, YE Yun1, ZHUO Hui1, ZHANG Hui2,*( ), LUO Yingquan1,*(
), LUO Yingquan1,*( )
)
Received:2022-12-04
Revised:2023-03-03
Published:2023-07-15
Online:2023-03-21
Contact:
ZHANG Hui, LUO Yingquan
About author:摘要: 背景 阻塞性睡眠呼吸暂停低通气综合征(OSAHS)在高血压患者中患病率高,但诊断率低,其中心率变异性(HRV)和血压变异性(BPV)都是心血管事件相关预测因子,但目前关于OSAHS与高血压患者BPV和HRV内在联系的相关研究较少。 目的 本研究旨在探讨OSAHS对高血压患者HRV、BPV的影响,并开发和内、外部验证一种通过HRV和BPV相关指标预测高血压患者OSAHS患病风险的列线图。 方法 选取2018年1月—2020年12月在中南大学湘雅二医院收治的228例高血压患者作为研究对象,根据OSAHS诊断标准分为单纯高血压组(n=114)和高血压合并OSAHS组(n=114);另外收集2021年1—2月住院的34例高血压伴或不伴OSAHS患者作为独立的外部验证组。收集研究对象的一般资料(年龄、性别、BMI等)、平均血压水平〔夜间收缩压(nSBP)等〕、BPV相关指标〔夜间收缩压标准差(nSSD)、夜间舒张压标准差(nDSD)、24 h舒张压标准差(24 hDSD)等〕、血压昼夜节律、HRV相关指标〔RR间期平均值标准差(SDANN)、低频带(LF)等〕、多导睡眠监测(PSG)参数〔氧减指数(ODI)、睡眠呼吸暂停低通气指数(AHI)、最低血氧饱和度(MinSpO2)等〕。采用多元线性回归分析探究HRV和BPV相关影响因素;并绘制限制性立方样条图检验高血压患者平均血压水平、BPV和HRV相关指标与OSAHS患病风险的相关性;通过多因素Logistic回归分析高血压患者患OSAHS的影响因素,构建列线图预测模型,采用Bootstrap方法在检验内、外部组验证组在列线图模型中的性能;采用受试者工作特征(ROC)曲线评估内、外部验证组列线图对高血压患者OSAHS患病风险的预测价值,计算ROC曲线下面积(AUC)等指标。 结果 多元线性回归分析结果显示:BMI、ODI、MinSpO2是高血压合并OSAHS组患者nSSD、nDSD水平和HRV相关指标的独立影响因素(P<0.05);限制性立方样条模型结果显示BPV、HRV相关指标与发生OSAHS存在非线性相关(P<0.05),纳入多元Logistic回归分析后发现nSBP、nSSD、24 hDSD、SDANN、LF、年龄、BMI是高血压患者发生OSAHS的影响因素(P<0.05);以年龄、BMI、nSBP、nSSD、24 hDSD、SDANN、LF为预测因子构建列线图预测模型,Bootstrap方法验证结果显示,内、外部验证组的绝对误差分别为0.013、0.021,表明列线图模型的校准度良好。内、外部验证组列线图预测高血压患者OSAHS患病风险的AUC分别为0.861〔95%CI(0.818,0.919),P<0.001〕、0.744〔95%CI(0.691,0.839),P<0.001〕。 结论 OSAHS可增加高血压患者夜间BPV,降低HRV,HRV和BPV均与OSAHS病情严重程度密切相关,夜间缺氧或许更能引起血压和心率变化。本研究构建的列线图也许可用于高血压患者发生OSAHS风险的个体化预测,HRV和BPV参数或许是筛选OSAHS的有力工具。
| 组别 | 例数 | 一般资料 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 年龄( | 性别〔n(%)〕 | BMI ( | 空腹血糖( | 肌酐( | 总胆固醇( | 三酰甘油( | LDL-C( | HDL-C( | 高血压病程( | 服用降压药物种类( | |||
| 男 | 女 | ||||||||||||
| 单纯高血压组 | 114 | 60.6±12.8 | 78(68.4) | 36(31.6) | 23.5±5.0 | 4.9±0.7 | 71.4±19.3 | 4.3±1.1 | 2.1±1.3 | 2.8±1.1 | 1.1±0.3 | 9.6±9.1 | 1.4±0.6 |
| 高血压合并OSAHS组 | 114 | 57.4±12.9 | 90(78.9) | 24(21.1) | 26.8±3.9 | 5.1±1.2 | 73.9±18.8 | 4.1±1.2 | 2.4±1.2 | 2.8±1.0 | 1.0±0.2 | 10.2±7.5 | 1.5±0.7 |
| t(χ2)值 | 1.880 | 1.805a | 5.556 | 1.537 | 0.992 | 1.312 | 1.811 | 0 | 1.376 | 0.543 | 1.158 | ||
| P值 | 0.061 | 0.071 | <0.001 | 0.126 | 0.318 | 0.191 | 0.072 | 0.996 | 0.173 | 0.570 | 0.269 | ||
| 组别 | 平均血压水平( | BPV相关指标( | |||||||||||
| 24 hSBP | 24 hDBP | dSBP | dDBP | nSBP | nDBP | 24 hSSD | 24 hDSD | dSSD | dDSD | nSSD | nDSD | ||
| 单纯高血压组 | 132±8 | 68±4 | 133±13 | 77±8 | 121±8 | 66±6 | 11±3 | 8±2 | 11±5 | 10±3 | 10±5 | 9±4 | |
| 高血压合并OSAHS组 | 139±8 | 72+6 | 136±12 | 78±14 | 134±9 | 70±8 | 14±3 | 11+2 | 12±5 | 10±4 | 12±5 | 13±6 | |
| t(χ2)值 | 6.428 | 7.327 | 1.884 | 0.889 | 11.260 | 4.631 | 7.300 | 10.860 | 1.963 | 1.224 | 4.130 | 5.841 | |
| P值 | <0.001 | <0.001 | 0.069 | 0.336 | <0.001 | <0.001 | <0.001 | <0.001 | 0.056 | 0.280 | <0.001 | <0.001 | |
| 组别 | 血压昼夜节律〔n(%)〕 | HRV相关指标 | |||||||||||
| 时域指标( | 频域指标( | ||||||||||||
| 杓型 | 非杓型 | ||||||||||||
| SDNN | SDANN | RMSSD | LF | HF | LF/HF | ||||||||
| 单纯高血压组 | 72(63.2) | 42(36.8) | 119.6±12.6 | 124.8±15.7 | 29.1±8.6 | 463.2±174.8 | 254.9±63.7 | 1.97±0.27 | |||||
| 高血压合并OSAHS组 | 34(29.8) | 80(70.2) | 91.1±20.5 | 90.0±20.3 | 22.5±10.0 | 360.2±58.3 | 231.6±47.9 | 2.08±0.50 | |||||
| t(χ2)值 | 5.046a | 12.650 | 14.480 | 5.343 | 5.968 | 3.121 | 2.067 | ||||||
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.002 | 0.039 | ||||||
表1 单纯高血压组与高血压合并OSAHS组患者临床资料比较
Table 1 Comparison of clinical data between hypertension patients with and without OSAHS
| 组别 | 例数 | 一般资料 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 年龄( | 性别〔n(%)〕 | BMI ( | 空腹血糖( | 肌酐( | 总胆固醇( | 三酰甘油( | LDL-C( | HDL-C( | 高血压病程( | 服用降压药物种类( | |||
| 男 | 女 | ||||||||||||
| 单纯高血压组 | 114 | 60.6±12.8 | 78(68.4) | 36(31.6) | 23.5±5.0 | 4.9±0.7 | 71.4±19.3 | 4.3±1.1 | 2.1±1.3 | 2.8±1.1 | 1.1±0.3 | 9.6±9.1 | 1.4±0.6 |
| 高血压合并OSAHS组 | 114 | 57.4±12.9 | 90(78.9) | 24(21.1) | 26.8±3.9 | 5.1±1.2 | 73.9±18.8 | 4.1±1.2 | 2.4±1.2 | 2.8±1.0 | 1.0±0.2 | 10.2±7.5 | 1.5±0.7 |
| t(χ2)值 | 1.880 | 1.805a | 5.556 | 1.537 | 0.992 | 1.312 | 1.811 | 0 | 1.376 | 0.543 | 1.158 | ||
| P值 | 0.061 | 0.071 | <0.001 | 0.126 | 0.318 | 0.191 | 0.072 | 0.996 | 0.173 | 0.570 | 0.269 | ||
| 组别 | 平均血压水平( | BPV相关指标( | |||||||||||
| 24 hSBP | 24 hDBP | dSBP | dDBP | nSBP | nDBP | 24 hSSD | 24 hDSD | dSSD | dDSD | nSSD | nDSD | ||
| 单纯高血压组 | 132±8 | 68±4 | 133±13 | 77±8 | 121±8 | 66±6 | 11±3 | 8±2 | 11±5 | 10±3 | 10±5 | 9±4 | |
| 高血压合并OSAHS组 | 139±8 | 72+6 | 136±12 | 78±14 | 134±9 | 70±8 | 14±3 | 11+2 | 12±5 | 10±4 | 12±5 | 13±6 | |
| t(χ2)值 | 6.428 | 7.327 | 1.884 | 0.889 | 11.260 | 4.631 | 7.300 | 10.860 | 1.963 | 1.224 | 4.130 | 5.841 | |
| P值 | <0.001 | <0.001 | 0.069 | 0.336 | <0.001 | <0.001 | <0.001 | <0.001 | 0.056 | 0.280 | <0.001 | <0.001 | |
| 组别 | 血压昼夜节律〔n(%)〕 | HRV相关指标 | |||||||||||
| 时域指标( | 频域指标( | ||||||||||||
| 杓型 | 非杓型 | ||||||||||||
| SDNN | SDANN | RMSSD | LF | HF | LF/HF | ||||||||
| 单纯高血压组 | 72(63.2) | 42(36.8) | 119.6±12.6 | 124.8±15.7 | 29.1±8.6 | 463.2±174.8 | 254.9±63.7 | 1.97±0.27 | |||||
| 高血压合并OSAHS组 | 34(29.8) | 80(70.2) | 91.1±20.5 | 90.0±20.3 | 22.5±10.0 | 360.2±58.3 | 231.6±47.9 | 2.08±0.50 | |||||
| t(χ2)值 | 5.046a | 12.650 | 14.480 | 5.343 | 5.968 | 3.121 | 2.067 | ||||||
| P值 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.002 | 0.039 | ||||||
| 组别 | 例数 | 年龄(岁) | BMI (kg/m2) | nSBP (mmHg) | nDBP (mmHg) | dSBP (mmHg) | dDBP (mmHg) | 24 hSBP (mmHg) | 24 hDBP (mmHg) | nSSD (mmHg) | nDSD (mmHg) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 轻度亚组 | 30 | 55.8±13.2 | 23.5±2.8 | 133±7 | 65±5 | 138±17 | 76±13 | 137±9 | 72±5 | 8±2 | 9±1 |
| 中度亚组 | 37 | 56.9±11.6 | 27.3±3.8 | 135±9 | 72±8 | 141±21 | 76±13 | 138±12 | 73±6 | 10±2a | 11±4a |
| 重度亚组 | 47 | 58.3±13.8 | 27.5±3.9ab | 134±10 | 71±8ab | 156±24ab | 88±13ab | 146±15ab | 74±8 | 16±5a | 16±7a |
| F值 | 1.076 | 46.340 | 1.666 | 28.520 | 23.290 | 32.200 | 17.300 | 2.886 | 165.000 | 85.540 | |
| P值 | 0.342 | <0.001 | 0.191 | <0.001 | <0.001 | <0.001 | <0.001 | 0.057 | <0.001 | <0.001 | |
| 组别 | dSSD (mmHg) | dDSD (mmHg) | 24 hSSD (mmHg) | 24 hDSD (mmHg) | SDNN (ms) | SDANN (ms) | RMSSD (ms) | LF (ms2) | HF (ms2) | LF/HF (ms2) | |
| 轻度亚组 | 12±5 | 9±3 | 13±1 | 11±2 | 114.4±38.0 | 106.3±30.8 | 19.5±6.1 | 390.2±63.1 | 322.1±44.3 | 1.7±0.1 | |
| 中度亚组 | 12±4 | 10±3 | 14±3 | 11±2 | 93.7±8.8a | 87.9±20.2 | 23.9±9.7a | 340.2±29.3a | 267.1±44.3a | 1.8±0.1a | |
| 重度亚组 | 13±5 | 12±5a | 15±4a | 11±2 | 82.1±11.3ab | 86.6±13.4ab | 25.9±8.3a | 307.9±33.5ab | 176.1±61.4ab | 1.9±0.1a | |
| F值 | 1.638 | 8.581 | 14.840 | 0.103 | 55.520 | 27.020 | 18.310 | 98.630 | 241.600 | 114.000 | |
| P值 | 0.196 | <0.001 | <0.001 | 0.902 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
表2 AHI标准下不同严重程度高血压合并OSAHS组患者年龄、BMI、平均血压水平、BPV和HRV相关指标比较(±s)
Table 2 Comparison of age,BMI,mean blood pressure,BPV and HRV related indices in hypertension patients with mild,moderate and severe OSAHS stratified by the level of AHI
| 组别 | 例数 | 年龄(岁) | BMI (kg/m2) | nSBP (mmHg) | nDBP (mmHg) | dSBP (mmHg) | dDBP (mmHg) | 24 hSBP (mmHg) | 24 hDBP (mmHg) | nSSD (mmHg) | nDSD (mmHg) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 轻度亚组 | 30 | 55.8±13.2 | 23.5±2.8 | 133±7 | 65±5 | 138±17 | 76±13 | 137±9 | 72±5 | 8±2 | 9±1 |
| 中度亚组 | 37 | 56.9±11.6 | 27.3±3.8 | 135±9 | 72±8 | 141±21 | 76±13 | 138±12 | 73±6 | 10±2a | 11±4a |
| 重度亚组 | 47 | 58.3±13.8 | 27.5±3.9ab | 134±10 | 71±8ab | 156±24ab | 88±13ab | 146±15ab | 74±8 | 16±5a | 16±7a |
| F值 | 1.076 | 46.340 | 1.666 | 28.520 | 23.290 | 32.200 | 17.300 | 2.886 | 165.000 | 85.540 | |
| P值 | 0.342 | <0.001 | 0.191 | <0.001 | <0.001 | <0.001 | <0.001 | 0.057 | <0.001 | <0.001 | |
| 组别 | dSSD (mmHg) | dDSD (mmHg) | 24 hSSD (mmHg) | 24 hDSD (mmHg) | SDNN (ms) | SDANN (ms) | RMSSD (ms) | LF (ms2) | HF (ms2) | LF/HF (ms2) | |
| 轻度亚组 | 12±5 | 9±3 | 13±1 | 11±2 | 114.4±38.0 | 106.3±30.8 | 19.5±6.1 | 390.2±63.1 | 322.1±44.3 | 1.7±0.1 | |
| 中度亚组 | 12±4 | 10±3 | 14±3 | 11±2 | 93.7±8.8a | 87.9±20.2 | 23.9±9.7a | 340.2±29.3a | 267.1±44.3a | 1.8±0.1a | |
| 重度亚组 | 13±5 | 12±5a | 15±4a | 11±2 | 82.1±11.3ab | 86.6±13.4ab | 25.9±8.3a | 307.9±33.5ab | 176.1±61.4ab | 1.9±0.1a | |
| F值 | 1.638 | 8.581 | 14.840 | 0.103 | 55.520 | 27.020 | 18.310 | 98.630 | 241.600 | 114.000 | |
| P值 | 0.196 | <0.001 | <0.001 | 0.902 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 组别 | 例数 | 年龄(岁) | BMI (kg/m2) | nSBP (mmHg) | nDBP (mmHg) | dSBP (mmHg) | dDBP (mmHg) | 24 hSBP (mmHg) | 24 hDBP (mmHg) | nSSD (mmHg) | nDSD (mmHg) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 轻度亚组 | 28 | 56.7±12.8 | 26.3±4.7 | 132±9 | 70±7 | 143±21 | 79±13 | 139±12 | 74±13 | 9±2 | 10±4 |
| 中度亚组 | 35 | 56.4±12.2 | 26.6±3.9 | 134±9 | 70±7 | 148±17 | 82±12 | 134±12 | 72±12 | 9±2 | 9±3 |
| 重度亚组 | 51 | 60.0±13.7 | 26.7±3.7 | 138±12 | 71±9 | 141±21 | 77±14 | 138±11 | 72±5 | 14±5ab | 14±6ab |
| F值 | 2.727 | 0.291 | 1.152 | 0.170 | 0.982 | 0.691 | 0.134 | 1.197 | 81.540 | 41.970 | |
| P值 | 0.067 | 0.748 | 0.317 | 0.844 | 0.375 | 0.502 | 0.874 | 0.303 | <0.001 | <0.001 | |
| 组别 | dSSD (mmHg) | dDSD (mmHg) | 24 hSSD (mmHg) | 24 hDSD (mmHg) | SDNN (ms) | SDANN (ms) | RMSSD (ms) | LF (ms2) | HF (ms2) | LF/HF (ms2) | |
| 轻度亚组 | 11±5 | 11±3 | 16±4 | 11±2 | 102.7±18.6 | 93.9±29.0 | 24.0±5.5 | 372.8±62.9 | 282.6±40.8 | 1.9±0.1 | |
| 中度亚组 | 12±6 | 10±1 | 14±3 | 11±2 | 101.5±29.7 | 97.1±13.8 | 25.4±8.0 | 330.0±34.7a | 225.3±45.5a | 1.7±0.1 | |
| 重度亚组 | 13±5 | 10±4 | 14±3a | 11±2 | 86.5±18.1ab | 88.1±17.6 | 21.8±11.2 | 327.8±25.1a | 209.1±78.8a | 2.1±0.1a | |
| F值 | 4.298 | 0.928 | 12.510 | 0.267 | 17.910 | 4.307 | 2.632 | 235.800 | 57.304 | 456.000 | |
| P值 | 0.061 | 0.396 | <0.001 | 0.766 | <0.001 | 0.064 | 0.073 | <0.001 | <0.001 | <0.001 |
表3 MinSpO2标准下不同严重程度高血压合并OSAHS组患者年龄、BMI、平均血压水平、BPV和HRV相关指标比较(±s)
Table 3 Comparison of age,BMI,mean blood pressure,BPV and HRV related indices in hypertension patients with mild,moderate and severe OSAHS stratified by the level of MinSpO2
| 组别 | 例数 | 年龄(岁) | BMI (kg/m2) | nSBP (mmHg) | nDBP (mmHg) | dSBP (mmHg) | dDBP (mmHg) | 24 hSBP (mmHg) | 24 hDBP (mmHg) | nSSD (mmHg) | nDSD (mmHg) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 轻度亚组 | 28 | 56.7±12.8 | 26.3±4.7 | 132±9 | 70±7 | 143±21 | 79±13 | 139±12 | 74±13 | 9±2 | 10±4 |
| 中度亚组 | 35 | 56.4±12.2 | 26.6±3.9 | 134±9 | 70±7 | 148±17 | 82±12 | 134±12 | 72±12 | 9±2 | 9±3 |
| 重度亚组 | 51 | 60.0±13.7 | 26.7±3.7 | 138±12 | 71±9 | 141±21 | 77±14 | 138±11 | 72±5 | 14±5ab | 14±6ab |
| F值 | 2.727 | 0.291 | 1.152 | 0.170 | 0.982 | 0.691 | 0.134 | 1.197 | 81.540 | 41.970 | |
| P值 | 0.067 | 0.748 | 0.317 | 0.844 | 0.375 | 0.502 | 0.874 | 0.303 | <0.001 | <0.001 | |
| 组别 | dSSD (mmHg) | dDSD (mmHg) | 24 hSSD (mmHg) | 24 hDSD (mmHg) | SDNN (ms) | SDANN (ms) | RMSSD (ms) | LF (ms2) | HF (ms2) | LF/HF (ms2) | |
| 轻度亚组 | 11±5 | 11±3 | 16±4 | 11±2 | 102.7±18.6 | 93.9±29.0 | 24.0±5.5 | 372.8±62.9 | 282.6±40.8 | 1.9±0.1 | |
| 中度亚组 | 12±6 | 10±1 | 14±3 | 11±2 | 101.5±29.7 | 97.1±13.8 | 25.4±8.0 | 330.0±34.7a | 225.3±45.5a | 1.7±0.1 | |
| 重度亚组 | 13±5 | 10±4 | 14±3a | 11±2 | 86.5±18.1ab | 88.1±17.6 | 21.8±11.2 | 327.8±25.1a | 209.1±78.8a | 2.1±0.1a | |
| F值 | 4.298 | 0.928 | 12.510 | 0.267 | 17.910 | 4.307 | 2.632 | 235.800 | 57.304 | 456.000 | |
| P值 | 0.061 | 0.396 | <0.001 | 0.766 | <0.001 | 0.064 | 0.073 | <0.001 | <0.001 | <0.001 |
| 项目 | nSSD | nDSD | dSSD | dDSD | 24 hSSD | 24 hDSD |
|---|---|---|---|---|---|---|
| 年龄 | -0.063 | -0.103 | -0.179 | -0.180 | 0.157 | -0.047 |
| BMI | 0.470a | 0.507a | -0.107 | 0.029 | 0.179 | 0.015 |
| AHI | 0.568a | 0.457a | 0.032 | 0.113 | 0.074 | 0.074 |
| ODI | 0.962a | 0.797a | -0.056 | 0.057 | 0.082 | 0.092 |
| MinSpO2 | -0.833a | -0.703a | -0.015 | -0.051 | -0.013 | 0.009 |
| MeanSpO2 | -0.116 | -0.139 | -0.071 | -0.132 | 0.095 | -0.183 |
| 总呼吸紊乱时间 | 0.019 | 0.029 | 0.016 | 0.148 | -0.007 | -0.059 |
| 平均暂停时间 | -0.002 | 0.092 | -0.125 | 0.016 | 0.184 | -0.091 |
| 最长呼吸暂停时间 | 0.018 | 0.048 | -0.010 | 0.071 | 0.101 | -0.115 |
| 总呼吸暂停时间 | 0.038 | 0.046 | 0.016 | 0.125 | -0.004 | -0.067 |
| 总低通气时间 | -0.146 | -0.145 | -0.007 | 0.139 | -0.032 | 0.079 |
| 呼吸紊乱时长所占百分比 | 0.054 | 0.086 | -0.007 | 0.092 | -0.034 | -0.093 |
表4 高血压合并OSAHS组患者BPV相关指标与患者年龄、BMI、PSG参数的相关性分析(r值)
Table 4 Correlation analysis of BPV related indices with age,BMI and PSG parameters in hypertension patients with OSAHS
| 项目 | nSSD | nDSD | dSSD | dDSD | 24 hSSD | 24 hDSD |
|---|---|---|---|---|---|---|
| 年龄 | -0.063 | -0.103 | -0.179 | -0.180 | 0.157 | -0.047 |
| BMI | 0.470a | 0.507a | -0.107 | 0.029 | 0.179 | 0.015 |
| AHI | 0.568a | 0.457a | 0.032 | 0.113 | 0.074 | 0.074 |
| ODI | 0.962a | 0.797a | -0.056 | 0.057 | 0.082 | 0.092 |
| MinSpO2 | -0.833a | -0.703a | -0.015 | -0.051 | -0.013 | 0.009 |
| MeanSpO2 | -0.116 | -0.139 | -0.071 | -0.132 | 0.095 | -0.183 |
| 总呼吸紊乱时间 | 0.019 | 0.029 | 0.016 | 0.148 | -0.007 | -0.059 |
| 平均暂停时间 | -0.002 | 0.092 | -0.125 | 0.016 | 0.184 | -0.091 |
| 最长呼吸暂停时间 | 0.018 | 0.048 | -0.010 | 0.071 | 0.101 | -0.115 |
| 总呼吸暂停时间 | 0.038 | 0.046 | 0.016 | 0.125 | -0.004 | -0.067 |
| 总低通气时间 | -0.146 | -0.145 | -0.007 | 0.139 | -0.032 | 0.079 |
| 呼吸紊乱时长所占百分比 | 0.054 | 0.086 | -0.007 | 0.092 | -0.034 | -0.093 |
| 因变量 | 自变量 | B(95%CI) | SE | β | t值 | P值 |
|---|---|---|---|---|---|---|
| nSSD | BMI | 0.387(0.338,0.436) | 0.025 | 0.119 | 15.480 | <0.001 |
| ODI | 0.582(0.333,0.831) | 0.127 | 0.364 | 4.583 | <0.001 | |
| MinSpO2 | -0.934(-1.030,-0.838) | 0.049 | -0.627 | -19.061 | <0.001 | |
| nDSD | BMI | 0.529(0.460,0.598) | 0.035 | 0.147 | 15.114 | <0.001 |
| ODI | 0.653(0.416,0.890) | 0.121 | 0.482 | 5.397 | <0.001 | |
| MinSpO2 | -0.793(-0.911,-0.675) | 0.060 | -0.659 | -13.217 | <0.001 |
表5 高血压合并OSAHS组患者nSSD、nDSD水平影响因素的多元线性回归分析
Table 5 Multiple linear regression analysis of the factors associated with the levels of nSSD and nDSD in hypertension patients with OSAHS
| 因变量 | 自变量 | B(95%CI) | SE | β | t值 | P值 |
|---|---|---|---|---|---|---|
| nSSD | BMI | 0.387(0.338,0.436) | 0.025 | 0.119 | 15.480 | <0.001 |
| ODI | 0.582(0.333,0.831) | 0.127 | 0.364 | 4.583 | <0.001 | |
| MinSpO2 | -0.934(-1.030,-0.838) | 0.049 | -0.627 | -19.061 | <0.001 | |
| nDSD | BMI | 0.529(0.460,0.598) | 0.035 | 0.147 | 15.114 | <0.001 |
| ODI | 0.653(0.416,0.890) | 0.121 | 0.482 | 5.397 | <0.001 | |
| MinSpO2 | -0.793(-0.911,-0.675) | 0.060 | -0.659 | -13.217 | <0.001 |
| 项目 | SDNN | SDANN | RMSSD | LF | HF | LF/HF |
|---|---|---|---|---|---|---|
| 年龄 | -0.105 | -0.073 | 0.093 | 0.090 | 0.038 | 0.025 |
| BMI | -0.324a | -0.382a | -0.229a | -0.384a | -0.419a | 0.241a |
| AHI | -0.371a | -0.349a | -0.299a | -0.433a | -0.495a | 0.300a |
| ODI | -0.489a | -0.296a | -0.427a | -0.515a | -0.809a | 0.473a |
| MinSpO2 | 0.519a | 0.168 | 0.409a | 0.503a | 0.736a | -0.415a |
| MeanSpO2 | -0.163 | -0.065 | 0.011 | -0.018 | 0.023 | 0.071 |
| 总呼吸紊乱时间 | 0.042 | -0.045 | 0.154 | 0.115 | 0.023 | 0.013 |
| 平均暂停时间 | -0.084 | -0.111 | 0.066 | 0.068 | 0.006 | -0.061 |
| 最长呼吸暂停时间 | -0.055 | 0.038 | 0.098 | 0.051 | -0.042 | 0.103 |
| 总呼吸暂停时间 | 0.037 | -0.057 | 0.144 | 0.018 | 0.012 | 0.013 |
| 总低通气时间 | 0.023 | 0.104 | 0.040 | 0.080 | 0.102 | 0.005 |
| 呼吸紊乱时长所占百分比 | 0.029 | -0.023 | 0.155 | 0.122 | 0.003 | -0.016 |
表6 高血压合并OSAHS组患者HRV相关指标与年龄、BMI、PSG参数的相关性分析(r值)
Table 6 Correlation analysis of HRV related indices with age,BMI and PSG parameters in hypertension patients with OSAHS
| 项目 | SDNN | SDANN | RMSSD | LF | HF | LF/HF |
|---|---|---|---|---|---|---|
| 年龄 | -0.105 | -0.073 | 0.093 | 0.090 | 0.038 | 0.025 |
| BMI | -0.324a | -0.382a | -0.229a | -0.384a | -0.419a | 0.241a |
| AHI | -0.371a | -0.349a | -0.299a | -0.433a | -0.495a | 0.300a |
| ODI | -0.489a | -0.296a | -0.427a | -0.515a | -0.809a | 0.473a |
| MinSpO2 | 0.519a | 0.168 | 0.409a | 0.503a | 0.736a | -0.415a |
| MeanSpO2 | -0.163 | -0.065 | 0.011 | -0.018 | 0.023 | 0.071 |
| 总呼吸紊乱时间 | 0.042 | -0.045 | 0.154 | 0.115 | 0.023 | 0.013 |
| 平均暂停时间 | -0.084 | -0.111 | 0.066 | 0.068 | 0.006 | -0.061 |
| 最长呼吸暂停时间 | -0.055 | 0.038 | 0.098 | 0.051 | -0.042 | 0.103 |
| 总呼吸暂停时间 | 0.037 | -0.057 | 0.144 | 0.018 | 0.012 | 0.013 |
| 总低通气时间 | 0.023 | 0.104 | 0.040 | 0.080 | 0.102 | 0.005 |
| 呼吸紊乱时长所占百分比 | 0.029 | -0.023 | 0.155 | 0.122 | 0.003 | -0.016 |
| 因变量 | 自变量 | B(95%CI) | SE | β | t值 | P值 |
|---|---|---|---|---|---|---|
| SDNN | BMI | -0.290(-0.449,-0.131) | 0.081 | -0.370 | -3.580 | 0.001 |
| ODI | -0.613(-0.846,-0.379) | 0.119 | -0.491 | -5.151 | <0.001 | |
| MinSpO2 | 0.539(0.443,0.635) | 0.049 | 0.553 | 11.000 | <0.001 | |
| SDANN | BMI | -0.582(-0.737,-0.427) | 0.079 | -0.382 | -7.367 | <0.001 |
| ODI | 0.724(0.434,1.014) | 0.148 | 0.503 | 4.892 | <0.001 | |
| MinSpO2 | 0.432(0.040,0.824) | 0.036 | 0.489 | 12.000 | <0.001 | |
| RMSSD | BMI | 0.159(-0.325,0.643) | 0.247 | 0.022 | 0.644 | 0.521 |
| ODI | -0.743(-0.829,-0.657) | 0.044 | -0.438 | -16.886 | <0.001 | |
| MinSpO2 | 0.139(-0.057,0.335) | 0.100 | 0.081 | 1.390 | 0.167 | |
| LF | BMI | -0.539(-0.802,-0.276) | 1.343 | -0.331 | -0.401 | 0.689 |
| ODI | 0.638(-2.067,3.342) | 1.380 | 0.484 | 0.462 | 0.645 | |
| MinSpO2 | 0.642(0.349,0.934) | 0.149 | 0.465 | 4.309 | <0.001 | |
| HF | BMI | -0.568(-0.789,-0.307) | 0.123 | -0.248 | -4.618 | <0.001 |
| ODI | -0.483(-0.548,-0.417) | 0.033 | -0.238 | -14.636 | <0.001 | |
| MinSpO2 | 0.647(0.298,0.996) | 0.178 | 0.630 | 3.635 | <0.001 |
表7 高血压合并OSAHS组患者HRV影响因素的多元线性回归分析
Table 7 Multiple linear regression analysis of associated factors of HRV in hypertension patients with OSAHS
| 因变量 | 自变量 | B(95%CI) | SE | β | t值 | P值 |
|---|---|---|---|---|---|---|
| SDNN | BMI | -0.290(-0.449,-0.131) | 0.081 | -0.370 | -3.580 | 0.001 |
| ODI | -0.613(-0.846,-0.379) | 0.119 | -0.491 | -5.151 | <0.001 | |
| MinSpO2 | 0.539(0.443,0.635) | 0.049 | 0.553 | 11.000 | <0.001 | |
| SDANN | BMI | -0.582(-0.737,-0.427) | 0.079 | -0.382 | -7.367 | <0.001 |
| ODI | 0.724(0.434,1.014) | 0.148 | 0.503 | 4.892 | <0.001 | |
| MinSpO2 | 0.432(0.040,0.824) | 0.036 | 0.489 | 12.000 | <0.001 | |
| RMSSD | BMI | 0.159(-0.325,0.643) | 0.247 | 0.022 | 0.644 | 0.521 |
| ODI | -0.743(-0.829,-0.657) | 0.044 | -0.438 | -16.886 | <0.001 | |
| MinSpO2 | 0.139(-0.057,0.335) | 0.100 | 0.081 | 1.390 | 0.167 | |
| LF | BMI | -0.539(-0.802,-0.276) | 1.343 | -0.331 | -0.401 | 0.689 |
| ODI | 0.638(-2.067,3.342) | 1.380 | 0.484 | 0.462 | 0.645 | |
| MinSpO2 | 0.642(0.349,0.934) | 0.149 | 0.465 | 4.309 | <0.001 | |
| HF | BMI | -0.568(-0.789,-0.307) | 0.123 | -0.248 | -4.618 | <0.001 |
| ODI | -0.483(-0.548,-0.417) | 0.033 | -0.238 | -14.636 | <0.001 | |
| MinSpO2 | 0.647(0.298,0.996) | 0.178 | 0.630 | 3.635 | <0.001 |
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | -0.53 | 0.015 | 4.478 | 0.035 | 1.04(1.01,1.06) |
| BMI | 1.722 | 0.082 | 5.824 | 0.014 | 1.13(1.07,1.31) |
| nSSD | 1.543 | 0.214 | 9.295 | 0.002 | 1.62(1.20,2.19) |
| SDANN | 0.770 | 0.015 | 7.715 | 0.005 | 0.95(0.92,0.98) |
| nSBP | 1.542 | 0.061 | 11.243 | <0.001 | 1.22(1.10,1.36) |
| 24 hDSD | 0.052 | 0.332 | 9.931 | <0.001 | 2.09(1.44,3.05) |
| LF | 1.070 | 0.006 | 10.246 | <0.001 | 0.97(0.96,0.99) |
表8 高血压患者发生OSAHS影响因素的多因素Logistic回归分析
Table 8 Multivariate Logistic regression analysis on the associated factors of OSAHS in hypertensive patients
| 变量 | B | SE | Wald χ2值 | P值 | OR(95%CI) |
|---|---|---|---|---|---|
| 年龄 | -0.53 | 0.015 | 4.478 | 0.035 | 1.04(1.01,1.06) |
| BMI | 1.722 | 0.082 | 5.824 | 0.014 | 1.13(1.07,1.31) |
| nSSD | 1.543 | 0.214 | 9.295 | 0.002 | 1.62(1.20,2.19) |
| SDANN | 0.770 | 0.015 | 7.715 | 0.005 | 0.95(0.92,0.98) |
| nSBP | 1.542 | 0.061 | 11.243 | <0.001 | 1.22(1.10,1.36) |
| 24 hDSD | 0.052 | 0.332 | 9.931 | <0.001 | 2.09(1.44,3.05) |
| LF | 1.070 | 0.006 | 10.246 | <0.001 | 0.97(0.96,0.99) |
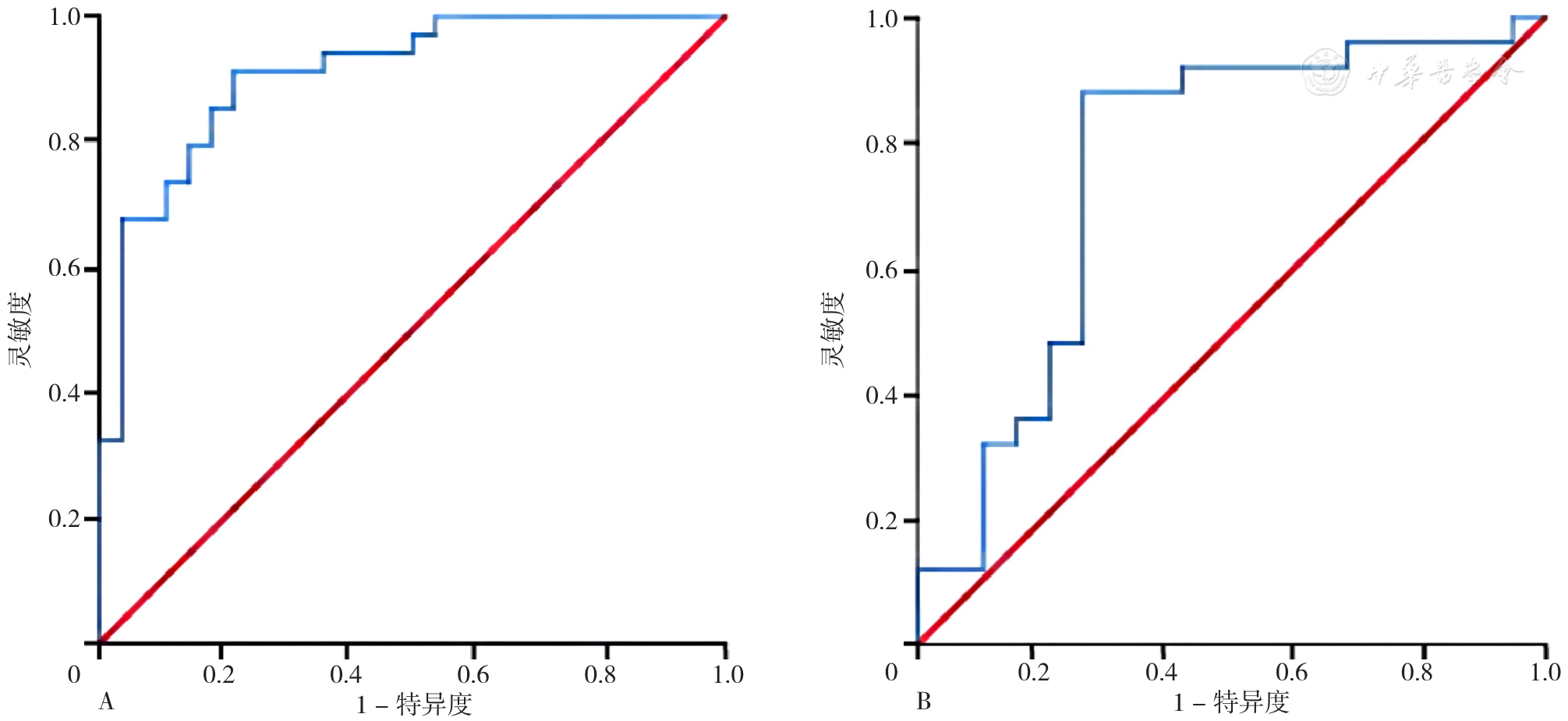
图2 内、外部验证组列线图预测高血压患者OSAHS患病风险的ROC曲线注:A表示内部验证组列线图的ROC曲线,B表示外部验证组列线图的ROC曲线。
Figure 2 ROC curves of the nomogram in predicting the risk of OSAHS in hypertensive patients in internal and external validation groups
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|
| [18] |
|
| [19] |
中国高血压防治指南修订委员会,高血压联盟(中国),中华医学会心血管病学分会,等. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志,2019,24(1):24-56. DOI:10.3969/j.issn.1007-5410.2019.01.002.
|
| [20] |
中华医学会呼吸病学分会睡眠呼吸障碍学组. 阻塞性睡眠呼吸暂停低通气综合征诊治指南(2011年修订版)[J]. 中华结核和呼吸杂志,2012,35(1):9-12. DOI:10.3760/cma.j.issn.1001-0939.2012.01.007.
|
| [21] |
|
| [22] |
|
| [23] |
|
| [24] |
|
| [25] |
|
| [26] |
|
| [27] |
|
| [28] |
|
| [29] |
|
| [30] |
|
| [31] |
|
| [32] |
|
| [33] |
|
| [34] |
|
| [35] |
|
| [36] |
|
| [37] |
|
| [38] |
|
| [39] |
|
| [1] | 常钰朋, 耿茜茜, 火睿, 孙侃, 常向云, 李军, 朱凌云, 董玉洁, 罗丽娜. 基于肾小球滤过率的肾上腺醛固酮瘤列线图预测模型的建立与验证研究[J]. 中国全科医学, 2024, 27(12): 1480-1486. |
| [2] | 金梦龙, 秦晓英, 马力亚·阿米提, 加孜呢·努尔拜, 李建新, 曹杰, 罗思富, 刘成, 张雨晨, 盖敏涛, 李艳鹏, 鲁向锋, 付真彦. 新疆哈萨克族血脂异常、高血压和糖尿病共病现状及影响因素研究[J]. 中国全科医学, 2024, 27(12): 1438-1444. |
| [3] | 曾凌枫, 张慧, 雷思, 卓慧, 叶云, 许琰, 罗荧荃. 《成年人阻塞性睡眠呼吸暂停低通气综合征筛查:美国预防临床服务指南工作组推荐声明》解读[J]. 中国全科医学, 2024, 27(12): 1412-1416. |
| [4] | 张幸, 董静, 郭怡, 徐建伟, 白雅敏, 刘敏, 张晓畅, 郭晓雷, 马吉祥, 孙昕霙. 基于PRECEDE模式的居民减盐行为影响因素的混合方法研究[J]. 中国全科医学, 2024, 27(10): 1221-1230. |
| [5] | 卢春远, 龙蓉, 毛永佳, 叶德鑫, 汪俊华, 张江萍. 35岁及以上社区高血压管理人群中血压变化轨迹及分布特征分析[J]. 中国全科医学, 2024, 27(10): 1201-1207. |
| [6] | 赵润泽, 孙小佳, Hernandez MELBA Marquez, 窦国睿. 光学相干断层成像评估高血压性视网膜病变神经元损伤应用价值的研究[J]. 中国全科医学, 2024, 27(09): 1082-1087. |
| [7] | 韩俊杰, 武迪, 陈志胜, 肖扬, 森干. 2型糖尿病患者并发糖尿病肾病风险的列线图预测模型与验证研究[J]. 中国全科医学, 2024, 27(09): 1054-1061. |
| [8] | 王畅, 权雅文, 王林峰, 李刚. 老年男性和女性血小板分布宽度与不同高血压亚型的相关性研究[J]. 中国全科医学, 2024, 27(08): 921-929. |
| [9] | 武淑琴, 王远涵, 郑凯元, 韩红娟, 康金秀, 余红梅. 恶性黑色素瘤患者的预后及影响因素研究[J]. 中国全科医学, 2024, 27(08): 942-947. |
| [10] | 袁仙仙, 李静, 王佳, 张可欣, 杨蕊华, 郑薇, 李光辉. 妊娠期血脂异常患病率及妊娠早期血脂水平预测价值研究[J]. 中国全科医学, 2024, 27(06): 670-678. |
| [11] | 庞爱梅, 高伟, 张恒, 蒲双双, 郭莉莉, 范子荣, 刘海霞, 刘瑞霞. 社区H型高血压患者药物基因作用靶点多态性分布及叶酸联合维生素D干预效果研究[J]. 中国全科医学, 2024, 27(06): 704-710. |
| [12] | 孙星河, 汪洋, 康俊萍, 刘小慧. 原发性高血压患者利用点尿钠估测24 h尿钠水平准确性的验证[J]. 中国全科医学, 2024, 27(06): 685-691. |
| [13] | 李雅萍, 李霞. 代谢综合征与阿尔茨海默病的相关性及机制研究进展[J]. 中国全科医学, 2024, 27(03): 268-272. |
| [14] | 代愉恒, 高畅, 梁新袖, 卢莎, 华雯, 郑钜圣, 胡文胜. 妊娠期糖尿病患者肠道菌群特征与妊娠期高血压疾病的关联研究[J]. 中国全科医学, 2024, 27(02): 156-162. |
| [15] | 姚琳, 尚丹梅, 赵慧, 刘新宇, 刘永伟, 姜涌. 移动网络在社区老年高血压管理中的效果及满意度调查[J]. 中国全科医学, 2024, 27(01): 85-90. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





