中国全科医学 ›› 2022, Vol. 25 ›› Issue (30): 3834-3842.DOI: 10.12114/j.issn.1007-9572.2022.0452
所属专题: 泌尿系统疾病最新文章合集; 胰腺炎最新文章合集
• 论著·医学循证 • 上一篇
陈美颖1, 陈木欣1, 王明欣1, 郑婵美2, 蔡玩珠2, 梁爱新2, 周春姣2,*( )
)
收稿日期:2022-06-01
修回日期:2022-07-18
出版日期:2022-10-20
发布日期:2022-08-04
通讯作者:
周春姣
基金资助:
Meiying CHEN1, Muxin CHEN1, Mingxin WANG1, Chanmei ZHENG2, Wanzhu CAI2, Aixin LIANG2, Chunjiao ZHOU2,*( )
)
Received:2022-06-01
Revised:2022-07-18
Published:2022-10-20
Online:2022-08-04
Contact:
Chunjiao ZHOU
About author:摘要: 背景 急性肾损伤是重症急性胰腺炎常见并发症之一,是重症急性胰腺炎患者预后不良的重要危险因素。防治重症急性胰腺炎患者并发急性肾损伤形势严峻,早期评估、干预相关危险因素可以预防或延缓重症急性胰腺炎患者急性肾损伤的发生。 目的 系统分析重症急性胰腺炎患者发生急性肾损伤的危险因素。 方法 计算机检索PubMed、Embase、Cochrane Library、Web of Science、中国知网(CNKI)、万方数据知识服务平台(Wanfang Data)、维普网(CQVIP)和中国生物医学文献服务系统(SinoMed)中关于重症急性胰腺炎患者发生急性肾损伤危险因素的文献,检索时限均为建库至2022年1月。由两名研究者按照纳入和排除标准独立进行文献筛选、资料提取和质量评价后,采用RevMan 5.4和Stata 15.1软件进行Meta分析。 结果 共纳入21篇文献,总病例数为3 823例。Meta分析结果显示,男性〔OR=1.42,95%CI(1.21,1.68),P<0.001〕,有饮酒史〔OR=1.51,95%CI(1.14,2.01),P=0.004〕,急性生理与慢性健康(APACHE Ⅱ)评分〔MD=5.69,95%CI(2.95,8.44),P<0.001〕、Ranson评分〔MD=2.58,95%CI(2.27,2.88),P<0.001〕、CT严重指数(CTSI)评分〔MD=1.48,95%CI(0.17,2.80),P=0.030〕高,白细胞计数〔MD=0.96,95%CI(0.47,1.44),P<0.001〕、白介素33(IL-33)〔MD=28.36,95%CI(19.05,37.67),P<0.001〕、C反应蛋白(CRP)〔MD=17.38,95%CI(12.39,22.38),P<0.001〕、血肌酐(Scr)〔MD=49.50,95%CI(24.80,74.19),P<0.001〕、降钙素原(PCT)〔MD=6.74,95%CI(3.36,10.12),P<0.001〕、中性粒细胞明胶酶相关脂质运载蛋白(NGAL)〔MD=18.31,95%CI(11.82,24.80),P<0.001〕、乳酸〔MD=0.87,95%CI(0.27,1.46),P=0.004〕水平升高,合并低氧血症〔OR=9.42,95%CI(4.81,18.44),P<0.001〕、高血压〔OR=1.35,95%CI(1.06,1.72),P=0.010〕、糖尿病〔OR=1.56,95%CI(1.20,2.04),P<0.001〕、冠心病〔OR=3.20,95%CI(1.41,7.24),P=0.005〕,采用机械通气〔OR=5.00,95%CI(2.76,9.07),P<0.001〕,合并休克〔OR=11.60,95%CI(3.37,39.91),P<0.001〕、感染〔OR=5.78,95%CI(3.10,10.79),P<0.001〕、多器官功能障碍综合征(MODS)〔OR=7.28,95%CI(3.56,14.88),P<0.001〕、腹腔出血〔OR=5.51,95%CI(1.38,22.09),P=0.020〕、急性呼吸窘迫综合征(ARDS)〔OR=9.61,95%CI(4.14,22.27),P<0.001〕、腹腔间室综合征(ACS)〔OR=5.79,95%CI(3.75,8.93),P<0.001〕,ICU入住时间长〔MD=8.77,95%CI(2.76,14.79),P=0.004〕是重症急性胰腺炎患者发生急性肾损伤的危险因素。 结论 男性、有饮酒史,APACHE Ⅱ评分、Ranson评分、CTSI评分高,白细胞计数、IL-33、CRP、Scr、PCT、NGAL等炎性指标增高及乳酸水平升高,合并低氧血症、高血压、糖尿病、冠心病等基础疾病,采用机械通气,合并休克、感染、MODS、腹腔出血、ARDS、ACS,ICU入住时间长可能是重症急性胰腺炎患者发生急性肾损伤的危险因素。临床医护人员应根据这些危险因素,早期识别并干预发生急性肾损伤的高危患者,降低SAP患者并发急性肾损伤的发生率与死亡率。
| 序号 | 检索策略 |
|---|---|
| #1 | ("Pancreatitis,Acute Necrotizing"[Mesh])OR(((((((((((((Necrotizing Pancreatitis,Acute[Title/Abstract])OR(Pancreatitis Necrotising[Title/Abstract]))OR(Pancreatitis Necrotisings[Title/Abstract])) OR (Acute Necrotizing Pancreatitis[Title/Abstract]))OR(Pancreatitis Necrotizing[Title/Abstract]))OR(Pancreatitis Necrotizings[Title/Abstract]))OR(Pancreatic Necrosis[Title/Abstract]))OR(Necrosis,Pancreatic[Title/Abstract]))OR(Pancreatic Necroses[Title/Abstract]))OR(Hemorrhagic Necrotic Pancreatitis[Title/Abstract]))OR(Hemorrhagic Necrotic Pancreatitides[Title/Abstract]))OR(Necrotic Pancreatitis,Hemorrhagic[Title/Abstract]))OR(Pancreatitis,Hemorrhagic Necrotic[Title/Abstract])) |
| #2 | ("Acute Kidney Injury"[Mesh])OR(((((((((((((((((((((((Acute Kidney Injuries[Title/Abstract]) OR (Kidney Injuries,Acute[Title/Abstract]))OR(Kidney Injury,Acute[Title/Abstract]))OR(Acute Renal Injury[Title/Abstract]))OR(Acute Renal Injuries[Title/Abstract]))OR(Renal Injuries,Acute[Title/Abstract]))OR(Renal Injury,Acute[Title/Abstract]))OR(Renal Insufficiency,Acute[Title/Abstract]))OR(Acute Renal Insufficiencies[Title/Abstract]))OR(Renal Insufficiencies,Acute[Title/Abstract]))OR(Acute Renal Insufficiency[Title/Abstract]))OR(Kidney Insufficiency,Acute[Title/Abstract]))OR(Acute Kidney Insufficiencies[Title/Abstract]))OR(Kidney Insufficiencies,Acute[Title/Abstract]))OR(Acute Kidney Insufficiency[Title/Abstract]))OR(Kidney Failure,Acute[Title/Abstract]))OR(Acute Kidney Failures[Title/Abstract]))OR(Kidney Failures,Acute[Title/Abstract]))OR(Acute Renal Failure[Title/Abstract]))OR(Acute Renal Failures[Title/Abstract]))OR(Renal Failures,Acute[Title/Abstract]))OR(Renal Failure,Acute[Title/Abstract]))OR(Acute Kidney Failure[Title/Abstract])) |
| #3 | ("Risk Factors"[Mesh])OR((Factor,Risk[Title/Abstract])OR(Risk Factor[Title/Abstract])) |
| #4 | #1 AND #2 AND #3 |
表1 PubMed文献检索策略
Table 1 Strategy for searching articles about risk factors of acute kidney injury in patients with severe acute pancreatitis in PubMed
| 序号 | 检索策略 |
|---|---|
| #1 | ("Pancreatitis,Acute Necrotizing"[Mesh])OR(((((((((((((Necrotizing Pancreatitis,Acute[Title/Abstract])OR(Pancreatitis Necrotising[Title/Abstract]))OR(Pancreatitis Necrotisings[Title/Abstract])) OR (Acute Necrotizing Pancreatitis[Title/Abstract]))OR(Pancreatitis Necrotizing[Title/Abstract]))OR(Pancreatitis Necrotizings[Title/Abstract]))OR(Pancreatic Necrosis[Title/Abstract]))OR(Necrosis,Pancreatic[Title/Abstract]))OR(Pancreatic Necroses[Title/Abstract]))OR(Hemorrhagic Necrotic Pancreatitis[Title/Abstract]))OR(Hemorrhagic Necrotic Pancreatitides[Title/Abstract]))OR(Necrotic Pancreatitis,Hemorrhagic[Title/Abstract]))OR(Pancreatitis,Hemorrhagic Necrotic[Title/Abstract])) |
| #2 | ("Acute Kidney Injury"[Mesh])OR(((((((((((((((((((((((Acute Kidney Injuries[Title/Abstract]) OR (Kidney Injuries,Acute[Title/Abstract]))OR(Kidney Injury,Acute[Title/Abstract]))OR(Acute Renal Injury[Title/Abstract]))OR(Acute Renal Injuries[Title/Abstract]))OR(Renal Injuries,Acute[Title/Abstract]))OR(Renal Injury,Acute[Title/Abstract]))OR(Renal Insufficiency,Acute[Title/Abstract]))OR(Acute Renal Insufficiencies[Title/Abstract]))OR(Renal Insufficiencies,Acute[Title/Abstract]))OR(Acute Renal Insufficiency[Title/Abstract]))OR(Kidney Insufficiency,Acute[Title/Abstract]))OR(Acute Kidney Insufficiencies[Title/Abstract]))OR(Kidney Insufficiencies,Acute[Title/Abstract]))OR(Acute Kidney Insufficiency[Title/Abstract]))OR(Kidney Failure,Acute[Title/Abstract]))OR(Acute Kidney Failures[Title/Abstract]))OR(Kidney Failures,Acute[Title/Abstract]))OR(Acute Renal Failure[Title/Abstract]))OR(Acute Renal Failures[Title/Abstract]))OR(Renal Failures,Acute[Title/Abstract]))OR(Renal Failure,Acute[Title/Abstract]))OR(Acute Kidney Failure[Title/Abstract])) |
| #3 | ("Risk Factors"[Mesh])OR((Factor,Risk[Title/Abstract])OR(Risk Factor[Title/Abstract])) |
| #4 | #1 AND #2 AND #3 |
| 第一作者 | 发表年份(年) | 研究类型 | AKI诊断标准 | 样本量(AKI组/非AKI组) | AKI发生率(%) | 暴露因素 | NOS评分 |
|---|---|---|---|---|---|---|---|
| 乔世峰[ | 2005 | 病例对照研究 | KDIGO | 246(31/215) | 12.6 | (1)(2)(6)(8)(9)(24)(32)(34)(38) | 8 |
| 周艳芳[ | 2007 | 病例对照研究 | KDIGO | 328(147/181) | 44.8 | (1)(6)(33)(34)(37)(38) | 7 |
| LI[ | 2010 | 病例对照研究 | KDIGO | 228(42/186) | 18.4 | (1)(2)(3)(6)(7)(9)(10)(11)(12)(24)(25)(26)(38) | 7 |
| WU[ | 2014 | 病例对照研究 | KDIGO | 245(43/202) | 17.6 | (2)(3)(4)(26)(28)(29) | 8 |
| 黄致远[ | 2014 | 病例对照研究 | KDIGO | 245(43/202) | 17.6 | (1)(2)(3)(4)(5)(26)(28)(29)(37)(39) | 8 |
| KUMAR[ | 2015 | 病例对照研究 | KDIGO | 72(14/58) | 19.4 | (1)(3)(9)(28)(29)(33) | 8 |
| 周海洋[ | 2015 | 病例对照研究 | KDIGO | 75(25/50) | 33.3 | (20)(21) | 8 |
| 王逸平[ | 2017 | 病例对照研究 | KDIGO | 108(54/54) | 50.0 | (1)(2)(3)(6)(10)(11)(13)(15)(16)(23)(27)(28)(29)(30)(31)(32)(33)(38)(39) | 8 |
| WANG[ | 2018 | 病例对照研究 | KDIGO | 105(48/57) | 45.7 | (1)(2)(3)(17)(20)(25)(27) | 7 |
| 覃凌燕[ | 2018 | 病例对照研究 | KDIGO | 289(63/226) | 21.8 | (1)(2)(16)(25)(27)(32)(39) | 8 |
| 林云霞[ | 2018 | 病例对照研究 | KDIGO | 308(83/225) | 27.0 | (1)(2)(3)(4)(6)(8)(10)(11)(16)(17)(28)(29) | 8 |
| MAO[ | 2019 | 病例对照研究 | KDIGO | 145(26/119) | 17.9 | (2)(5) | 8 |
| 吴自谦[ | 2020 | 病例对照研究 | KDIGO | 105(32/73) | 30.5 | (1)(2)(25)(27)(28)(29)(30)(31)(32)(36) | 8 |
| 牛美红[ | 2020 | 病例对照研究 | KDIGO | 130(30/100) | 23.0 | (2)(7)(32)(33)(35)(36)(37)(38) | 7 |
| 吴敏[ | 2020 | 病例对照研究 | KDIGO | 291(95/196) | 32.6 | (2)(13)(25)(27) | 8 |
| 于晓燕[ | 2020 | 病例对照研究 | KDIGO | 121(35/86) | 28.9 | (2)(8)(14)(18)(19)(20)(21)(22) | 7 |
| 李秀娟[ | 2021 | 病例对照研究 | KDIGO | 130(24/106) | 18.5 | (2)(3)(4)(6)(9)(13)(14)(15)(16)(28)(29)(33)(35) | 8 |
| 黄鲜[ | 2021 | 病例对照研究 | KDIGO | 163(48/115) | 29.4 | (1)(2)(8)(14)(18)(19)(20)(21)(22) | 8 |
| 周双炉[ | 2022 | 病例对照研究 | KDIGO | 120(57/63) | 47.5 | (1)(2)(3)(4)(5)(6)(12)(16)(21)(23)(25)(27)(28)(29) | 8 |
| 李峰[ | 2022 | 病例对照研究 | KDIGO | 174(52/122) | 29.9 | (1)(2)(14)(19)(20)(28)(29) | 8 |
| 宋微[ | 2022 | 病例对照研究 | KDIGO | 195(57/138) | 29.2 | (1)(2)(5)(20)(28)(29) | 8 |
表2 纳入文献的基本特征
Table 2 Basic characteristics of included literature
| 第一作者 | 发表年份(年) | 研究类型 | AKI诊断标准 | 样本量(AKI组/非AKI组) | AKI发生率(%) | 暴露因素 | NOS评分 |
|---|---|---|---|---|---|---|---|
| 乔世峰[ | 2005 | 病例对照研究 | KDIGO | 246(31/215) | 12.6 | (1)(2)(6)(8)(9)(24)(32)(34)(38) | 8 |
| 周艳芳[ | 2007 | 病例对照研究 | KDIGO | 328(147/181) | 44.8 | (1)(6)(33)(34)(37)(38) | 7 |
| LI[ | 2010 | 病例对照研究 | KDIGO | 228(42/186) | 18.4 | (1)(2)(3)(6)(7)(9)(10)(11)(12)(24)(25)(26)(38) | 7 |
| WU[ | 2014 | 病例对照研究 | KDIGO | 245(43/202) | 17.6 | (2)(3)(4)(26)(28)(29) | 8 |
| 黄致远[ | 2014 | 病例对照研究 | KDIGO | 245(43/202) | 17.6 | (1)(2)(3)(4)(5)(26)(28)(29)(37)(39) | 8 |
| KUMAR[ | 2015 | 病例对照研究 | KDIGO | 72(14/58) | 19.4 | (1)(3)(9)(28)(29)(33) | 8 |
| 周海洋[ | 2015 | 病例对照研究 | KDIGO | 75(25/50) | 33.3 | (20)(21) | 8 |
| 王逸平[ | 2017 | 病例对照研究 | KDIGO | 108(54/54) | 50.0 | (1)(2)(3)(6)(10)(11)(13)(15)(16)(23)(27)(28)(29)(30)(31)(32)(33)(38)(39) | 8 |
| WANG[ | 2018 | 病例对照研究 | KDIGO | 105(48/57) | 45.7 | (1)(2)(3)(17)(20)(25)(27) | 7 |
| 覃凌燕[ | 2018 | 病例对照研究 | KDIGO | 289(63/226) | 21.8 | (1)(2)(16)(25)(27)(32)(39) | 8 |
| 林云霞[ | 2018 | 病例对照研究 | KDIGO | 308(83/225) | 27.0 | (1)(2)(3)(4)(6)(8)(10)(11)(16)(17)(28)(29) | 8 |
| MAO[ | 2019 | 病例对照研究 | KDIGO | 145(26/119) | 17.9 | (2)(5) | 8 |
| 吴自谦[ | 2020 | 病例对照研究 | KDIGO | 105(32/73) | 30.5 | (1)(2)(25)(27)(28)(29)(30)(31)(32)(36) | 8 |
| 牛美红[ | 2020 | 病例对照研究 | KDIGO | 130(30/100) | 23.0 | (2)(7)(32)(33)(35)(36)(37)(38) | 7 |
| 吴敏[ | 2020 | 病例对照研究 | KDIGO | 291(95/196) | 32.6 | (2)(13)(25)(27) | 8 |
| 于晓燕[ | 2020 | 病例对照研究 | KDIGO | 121(35/86) | 28.9 | (2)(8)(14)(18)(19)(20)(21)(22) | 7 |
| 李秀娟[ | 2021 | 病例对照研究 | KDIGO | 130(24/106) | 18.5 | (2)(3)(4)(6)(9)(13)(14)(15)(16)(28)(29)(33)(35) | 8 |
| 黄鲜[ | 2021 | 病例对照研究 | KDIGO | 163(48/115) | 29.4 | (1)(2)(8)(14)(18)(19)(20)(21)(22) | 8 |
| 周双炉[ | 2022 | 病例对照研究 | KDIGO | 120(57/63) | 47.5 | (1)(2)(3)(4)(5)(6)(12)(16)(21)(23)(25)(27)(28)(29) | 8 |
| 李峰[ | 2022 | 病例对照研究 | KDIGO | 174(52/122) | 29.9 | (1)(2)(14)(19)(20)(28)(29) | 8 |
| 宋微[ | 2022 | 病例对照研究 | KDIGO | 195(57/138) | 29.2 | (1)(2)(5)(20)(28)(29) | 8 |
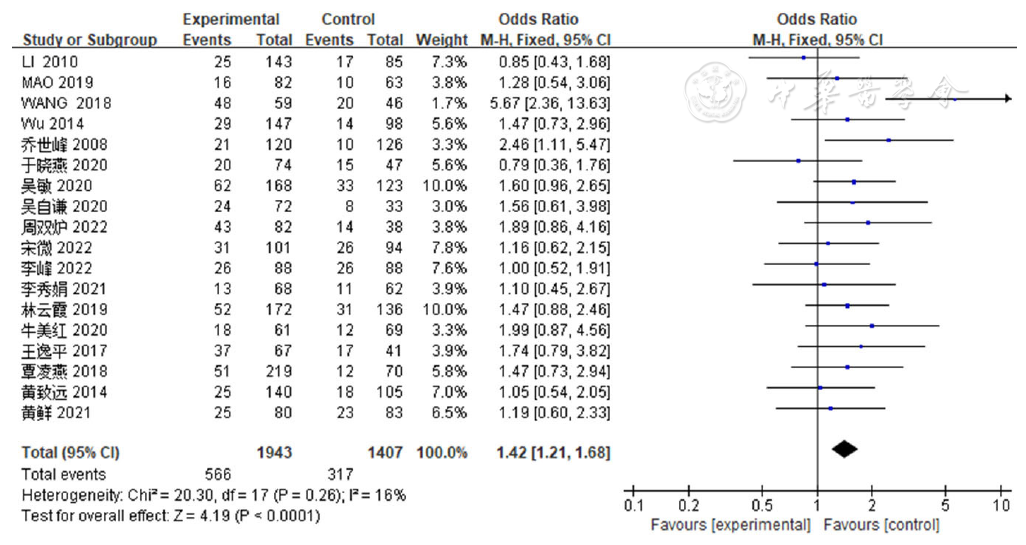
图2 性别对SAP患者并发AKI影响的Meta分析注:SAP=重症急性胰腺炎,AKI=急性肾损伤
Figure 2 Meta-analysis of the association of sex with acute kidney injury in patients with severe acute pancreatitis
| 危险因素 | 纳入研究(项) | 患者例数(例) | 异质性检验 | 效应模型 | 效应值 | 95%CI | P值 | ||
|---|---|---|---|---|---|---|---|---|---|
| I2值(%) | P值 | ||||||||
| 一般因素 | 性别 | 18[ | 3 350 | 16 | 0.260 | 固定 | OR=1.42 | (1.21,1.68) | <0.001 |
| 饮酒史 | 9[ | 1 559 | 22 | 0.250 | 固定 | OR=1.51 | (1.14,2.01) | 0.004 | |
| 客观指标因素 | APACHE Ⅱ评分 | 7[ | 1 468 | 95 | <0.001 | 随机 | MD=5.69 | (2.95,8.44) | <0.001 |
| Ranson评分 | 4[ | 838 | 76 | 0.005 | 随机 | MD=2.58 | (2.27,2.88) | <0.001 | |
| CTSI评分 | 2[ | 413 | 94 | <0.001 | 随机 | MD=1.48 | (0.17,2.80) | 0.030 | |
| 白细胞计数 | 5[ | 955 | 17 | 0.310 | 固定 | MD=0.96 | (0.47,1.44) | <0.001 | |
| IL-33 | 2[ | 284 | 0 | 0.920 | 固定 | MD=28.36 | (19.05,37.67) | <0.001 | |
| CRP | 3[ | 458 | 83 | 0.003 | 随机 | MD=17.38 | (12.39,22.38) | <0.001 | |
| Scr | 6[ | 833 | 98 | <0.001 | 随机 | MD=49.50 | (24.80,74.19) | <0.001 | |
| PCT | 4[ | 479 | 96 | <0.001 | 随机 | MD=6.74 | (3.36,10.12) | <0.001 | |
| NGAL | 2[ | 284 | 0 | 0.770 | 固定 | MD=18.31 | (11.82,24.80) | <0.001 | |
| 乳酸 | 2[ | 228 | 60 | 0.110 | 随机 | MD=0.87 | (0.27,1.46) | 0.004 | |
| 疾病因素 | 低氧血症 | 2[ | 474 | 15 | 0.280 | 固定 | OR=9.42 | (4.81,18.44) | <0.001 |
| 高血压 | 10[ | 1 702 | 0 | 0.540 | 固定 | OR=1.35 | (1.06,1.72) | 0.010 | |
| 糖尿病 | 10[ | 1 702 | 0 | 0.880 | 固定 | OR=1.56 | (1.20,2.04) | <0.001 | |
| 冠心病 | 2[ | 213 | 0 | 0.700 | 固定 | OR=3.20 | (1.41,7.24) | 0.005 | |
| 治疗因素 | 机械通气 | 5[ | 878 | 60 | 0.040 | 随机 | OR=5.00 | (2.76,9.07) | <0.001 |
| 合并症 | 休克 | 5[ | 768 | 68 | 0.010 | 随机 | OR=11.60 | (3.37,39.91) | <0.001 |
| 感染 | 2[ | 574 | 0 | 0.720 | 固定 | OR=5.78 | (3.10,10.79) | <0.001 | |
| MODS | 2[ | 260 | 0 | 0.580 | 固定 | OR=7.28 | (3.56,14.88) | <0.001 | |
| 腹腔出血 | 2[ | 235 | 77 | 0.040 | 随机 | OR=5.51 | (1.38,22.09) | 0.020 | |
| ARDS | 3[ | 703 | 69 | 0.040 | 随机 | OR=9.61 | (4.14,22.27) | <0.001 | |
| ACS | 5[ | 1 040 | 0 | 0.940 | 固定 | OR=5.79 | (3.75,8.93) | <0.001 | |
| 其他 | ICU入住时间 | 3[ | 642 | 89 | <0.001 | 随机 | MD=8.77 | (2.76,14.79) | 0.004 |
表3 SAP患者并发AKI危险因素的Meta分析
Table 3 Meta-analysis of risk factors for acute kidney injury in patients with severe acute pancreatitis
| 危险因素 | 纳入研究(项) | 患者例数(例) | 异质性检验 | 效应模型 | 效应值 | 95%CI | P值 | ||
|---|---|---|---|---|---|---|---|---|---|
| I2值(%) | P值 | ||||||||
| 一般因素 | 性别 | 18[ | 3 350 | 16 | 0.260 | 固定 | OR=1.42 | (1.21,1.68) | <0.001 |
| 饮酒史 | 9[ | 1 559 | 22 | 0.250 | 固定 | OR=1.51 | (1.14,2.01) | 0.004 | |
| 客观指标因素 | APACHE Ⅱ评分 | 7[ | 1 468 | 95 | <0.001 | 随机 | MD=5.69 | (2.95,8.44) | <0.001 |
| Ranson评分 | 4[ | 838 | 76 | 0.005 | 随机 | MD=2.58 | (2.27,2.88) | <0.001 | |
| CTSI评分 | 2[ | 413 | 94 | <0.001 | 随机 | MD=1.48 | (0.17,2.80) | 0.030 | |
| 白细胞计数 | 5[ | 955 | 17 | 0.310 | 固定 | MD=0.96 | (0.47,1.44) | <0.001 | |
| IL-33 | 2[ | 284 | 0 | 0.920 | 固定 | MD=28.36 | (19.05,37.67) | <0.001 | |
| CRP | 3[ | 458 | 83 | 0.003 | 随机 | MD=17.38 | (12.39,22.38) | <0.001 | |
| Scr | 6[ | 833 | 98 | <0.001 | 随机 | MD=49.50 | (24.80,74.19) | <0.001 | |
| PCT | 4[ | 479 | 96 | <0.001 | 随机 | MD=6.74 | (3.36,10.12) | <0.001 | |
| NGAL | 2[ | 284 | 0 | 0.770 | 固定 | MD=18.31 | (11.82,24.80) | <0.001 | |
| 乳酸 | 2[ | 228 | 60 | 0.110 | 随机 | MD=0.87 | (0.27,1.46) | 0.004 | |
| 疾病因素 | 低氧血症 | 2[ | 474 | 15 | 0.280 | 固定 | OR=9.42 | (4.81,18.44) | <0.001 |
| 高血压 | 10[ | 1 702 | 0 | 0.540 | 固定 | OR=1.35 | (1.06,1.72) | 0.010 | |
| 糖尿病 | 10[ | 1 702 | 0 | 0.880 | 固定 | OR=1.56 | (1.20,2.04) | <0.001 | |
| 冠心病 | 2[ | 213 | 0 | 0.700 | 固定 | OR=3.20 | (1.41,7.24) | 0.005 | |
| 治疗因素 | 机械通气 | 5[ | 878 | 60 | 0.040 | 随机 | OR=5.00 | (2.76,9.07) | <0.001 |
| 合并症 | 休克 | 5[ | 768 | 68 | 0.010 | 随机 | OR=11.60 | (3.37,39.91) | <0.001 |
| 感染 | 2[ | 574 | 0 | 0.720 | 固定 | OR=5.78 | (3.10,10.79) | <0.001 | |
| MODS | 2[ | 260 | 0 | 0.580 | 固定 | OR=7.28 | (3.56,14.88) | <0.001 | |
| 腹腔出血 | 2[ | 235 | 77 | 0.040 | 随机 | OR=5.51 | (1.38,22.09) | 0.020 | |
| ARDS | 3[ | 703 | 69 | 0.040 | 随机 | OR=9.61 | (4.14,22.27) | <0.001 | |
| ACS | 5[ | 1 040 | 0 | 0.940 | 固定 | OR=5.79 | (3.75,8.93) | <0.001 | |
| 其他 | ICU入住时间 | 3[ | 642 | 89 | <0.001 | 随机 | MD=8.77 | (2.76,14.79) | 0.004 |
| 危险因素 | MD (OR)值(95%CI) | |
|---|---|---|
| 随机效应模型 | 固定效应模型 | |
| APACHE Ⅱ评分 | 5.69(2.95,8.44) | 5.15(4.55,5.75) |
| Ranson评分 | 2.58(2.27,2.88) | 2.75(2.65,2.85) |
| CTSI评分 | 1.48(0.17,2.80) | 1.72(1.43,2.01) |
| CRP | 17.38(12.39,22.38) | 19.30(17.50,21.10) |
| Scr | 49.50(24.80,74.19) | 12.27(8.77,15.76) |
| PCT | 6.74(3.36,10.12) | 3.42(2.83,4.01) |
| 乳酸 | 0.87(0.27,1.46) | 0.77(0.44,1.09) |
| 机械通气 | 5.00(2.76,9.07)a | 4.74(3.31,6.79) |
| 休克 | 11.60(3.37,39.91)a | 9.30(5.33,16.23) |
| 腹腔出血 | 5.51(1.38,22.09)a | 4.81(2.52,9.17) |
| ARDS | 9.61(4.14,22.27)a | 8.38(5.26,13.37) |
| ICU入住时间 | 8.77(2.76,14.79) | 8.64(6.83,10.45) |
表4 SAP患者并发AKI危险因素的敏感性分析
Table 4 Sensitivity analysis results of risk factors of acute kidney injury in severe acute pancreatitis
| 危险因素 | MD (OR)值(95%CI) | |
|---|---|---|
| 随机效应模型 | 固定效应模型 | |
| APACHE Ⅱ评分 | 5.69(2.95,8.44) | 5.15(4.55,5.75) |
| Ranson评分 | 2.58(2.27,2.88) | 2.75(2.65,2.85) |
| CTSI评分 | 1.48(0.17,2.80) | 1.72(1.43,2.01) |
| CRP | 17.38(12.39,22.38) | 19.30(17.50,21.10) |
| Scr | 49.50(24.80,74.19) | 12.27(8.77,15.76) |
| PCT | 6.74(3.36,10.12) | 3.42(2.83,4.01) |
| 乳酸 | 0.87(0.27,1.46) | 0.77(0.44,1.09) |
| 机械通气 | 5.00(2.76,9.07)a | 4.74(3.31,6.79) |
| 休克 | 11.60(3.37,39.91)a | 9.30(5.33,16.23) |
| 腹腔出血 | 5.51(1.38,22.09)a | 4.81(2.52,9.17) |
| ARDS | 9.61(4.14,22.27)a | 8.38(5.26,13.37) |
| ICU入住时间 | 8.77(2.76,14.79) | 8.64(6.83,10.45) |
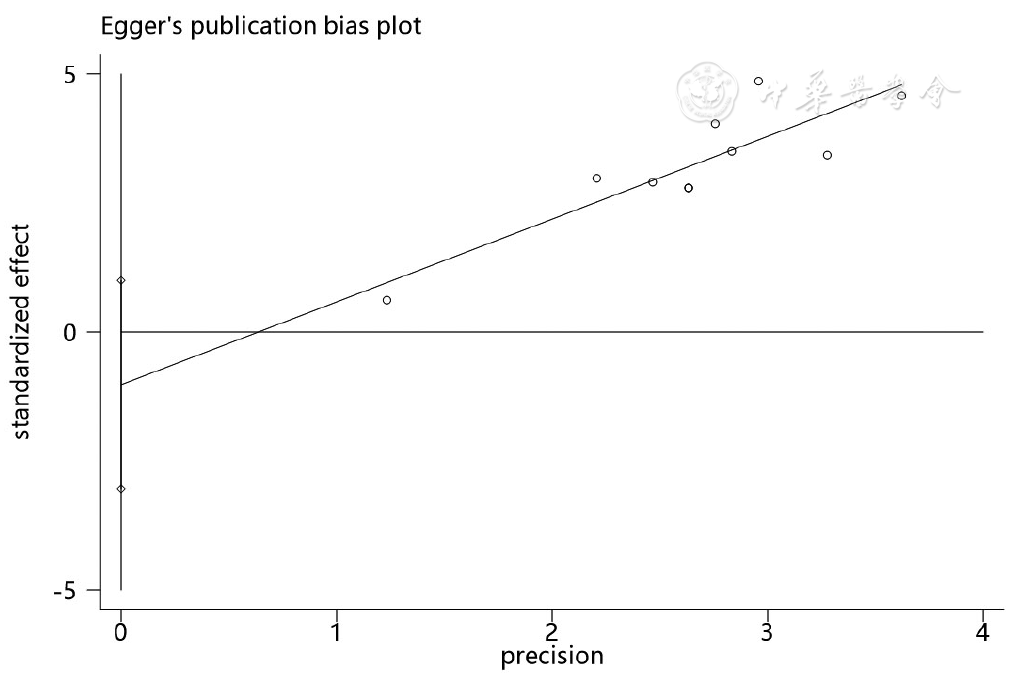
图3 高血压作为SAP患者并发AKI危险因素的Egger图
Figure 3 Egger's test assessing the publication bias of hypertension as a risk factor of acute kidney injury in severe acute pancreatitis
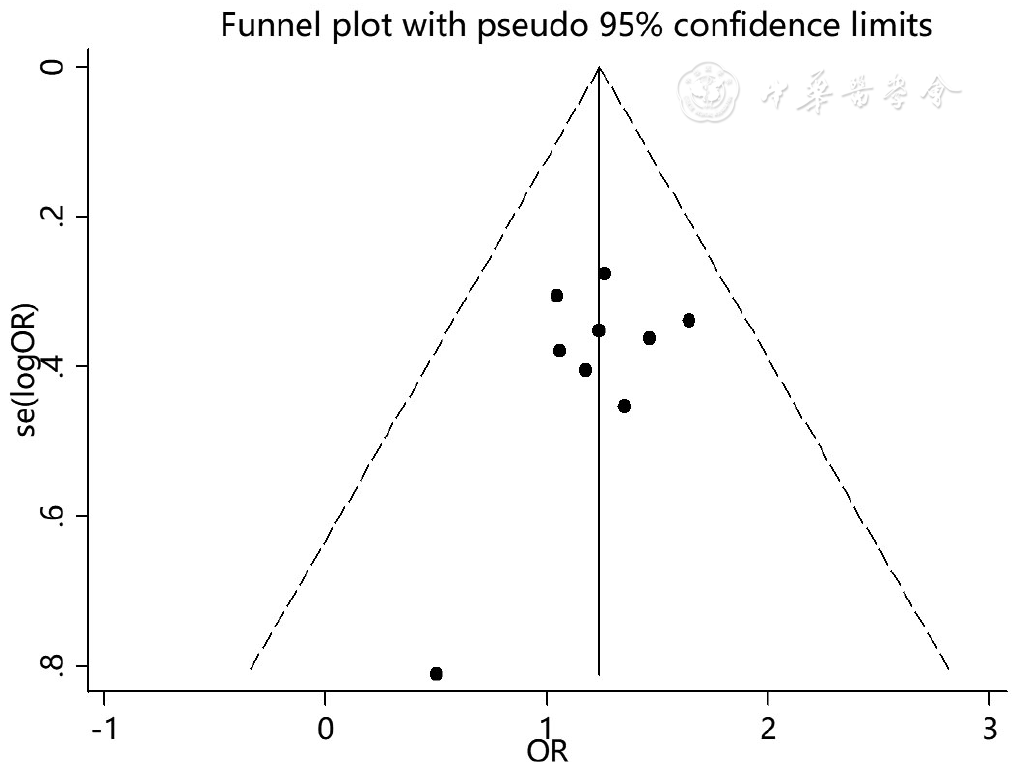
图4 高血压作为SAP患者并发AKI危险因素的漏斗图
Figure 4 Funnel plot assessing the publication bias of hypertension as a risk factor of acute kidney injury in severe acute pancreatitis
| [1] |
夏乐,李春华,沈佳庆.BISAP评分联合TG、MAP1-LC3对急性胰腺炎预后的预测价值[J]. 中国中西医结合消化杂志,2018,26(12):1009-1012. DOI:10.3969/j.issn.1671-038X.2018.12.08.
|
| [2] |
|
| [3] |
|
| [4] |
黄雯雪,陈春洁,孙艳. 急性胰腺炎相关危险因素、严重程度评估及临床护理研究进展[J]. 中国基层医药,2022,29(3):473-476. DOI:10.3760/cma.j.issn.1008-6706.2022.03.034.
|
| [5] |
|
| [6] |
|
| [7] |
杜雯雯,王晓星,陈文倩,等. RIFLE、AKIN和KDIGO急性肾损伤诊断标准在肺移植术后的应用比较[J]. 中国血液净化,2021,20(2):95-98,141. DOI:10.3969/j.issn.1671-4091.2021.02.006.
|
| [8] |
|
| [9] |
乔世峰,孙家邦,李非,等. 重症急性胰腺炎急性肾功能衰竭临床危险因素及其预防[J]. 中华肝胆外科杂志,2005,11(5):293-295. DOI:10.3760/cma.j.issn.1007-8118.2005.05.002.
|
| [10] |
周艳芳,许春进. 重症急性胰腺炎并发肾脏损害的临床研究[J]. 中国综合临床,2007,23(11):980-981. DOI:10.3760/cma.j.issn.1008-6315.2007.11.011.
|
| [11] |
|
| [12] |
|
| [13] |
黄致远,蔡逊,金炜东,等. 重症急性胰腺炎肾损伤危险因素分析[J]. 临床外科杂志,2014(12):919-921. DOI:10.3969/j.issn.1005-6483.2014.12.016.
|
| [14] |
|
| [15] |
周海洋,宁果豪,聂绍良. 降钙素原对重症急性胰腺炎合并急性肾损伤早期预测作用的研究[J]. 临床急诊杂志,2015,16(2):106-108. DOI:10.13201/j.issn.1009-5918.2015.02.008.
|
| [16] |
王逸平,刘向新,崔晓莉,等. 重症急性胰腺炎并发急性肾损伤临床特征及危险因素分析[J]. 交通医学,2017,31(5):473-476.
|
| [17] |
|
| [18] |
覃凌燕. 重症急性胰腺炎并急性肾损伤危险因素及预后分析[D]. 南宁:广西医科大学,2018.
|
| [19] |
林云霞,何晓彬,陈杰.重症急性胰腺炎并发急性肾衰竭的相关危险因素及预测模型[J]. 中国临床研究,2018,31(8):1043-1046. DOI:10.13429/j.cnki.cjcr.2018.08.008.
|
| [20] |
|
| [21] |
吴自谦,刘楠,万有栋,等. 重症急性胰腺炎影响肾功能恢复危险因素分析[J]. 中华急诊医学杂志,2020,29(9):1173-1177. DOI:10.3760/cma.j.issn.1671-0282.2020.09.007.
|
| [22] |
牛美红,郭继慧,赵丹. 老年重症急性胰腺炎患者并发急性肾损伤的影响因素[J]. 中国老年学杂志,2020,40(9):1859-1862. DOI:10.3969/j.issn.1005-9202.2020.09.022.
|
| [23] |
吴敏.重症急性胰腺炎合并急性肾损伤的临床特点及预后分析[D]. 重庆:重庆医科大学,2020.
|
| [24] |
于晓燕,赵腾. IL-33在预测重症急性胰腺炎患者发生急性肾损伤的临床效能[J]. 中国中西医结合肾病杂志,2020,21(1):37-39. DOI:10.3969/j.issn.1009-587X.2020.01.012.
|
| [25] |
李秀娟,黄坚,王楠,等. 重症急性胰腺炎患者并发急性肾损伤的危险因素分析[J]. 中国急救复苏与灾害医学杂志,2021,16(9):1011-1014. DOI:10.3969/j.issn.1673-6966.2021.09.013.
|
| [26] |
黄鲜,张丽涓,王平. 血清miR-10a、IL-33水平对重症急性胰腺炎患者并发急性肾损伤的预测价值[J]. 中国医药导报,2021,18(4):29-32.
|
| [27] |
周双炉,常玲,邢芳芳. PCT、NLR、N/LPR对重症急性胰腺炎并发急性肾损伤的预测价值[J]. 新医学,2022,53(2):133-137. DOI:10.3969/j.issn.0253-9802.2022.02.012.
|
| [28] |
李峰,刘春生. 全身免疫炎症指数对重症胰腺炎并发急性肾损伤早期预测价值的研究[J]. 临床急诊杂志,2022,23(2):100-105. DOI:10.13201/j.issn.1009-5918.2022.02.005.
|
| [29] |
宋微,李虹怡,吕洪波. 血清miR-21-3p、IL-18水平对重症急性胰腺炎患者急性肾损伤的预测价值[J]. 山东医药,2022,62(1):20-24. DOI:10.3969/j.issn.1002-266X.2022.01.005.
|
| [30] |
许承,苏江林. 重症急性胰腺炎并发急性肾衰竭的危险因素研究进展[J]. 西南国防医药,2018,28(5):492-494. DOI:10.3969/j.issn.1004-0188.2018.05.039.
|
| [31] |
|
| [32] |
陆任华,方燕,高嘉元,等. 住院患者急性肾损伤发病情况及危险因素分析[J]. 中国危重病急救医学,2011,23(7):413-417. DOI:10.3760/cma.j.issn.1003-0603.2011.07.010.
|
| [33] | |
| [34] |
李强,付君静,窦文广,等. CT评价系统联合血浆D-二聚体对重症急性胰腺炎预后的预测价值[J]. 中华实用诊断与治疗杂志,2020,34(10):1050-1053. DOI:10.13507/j.issn.1674-3474.2020.10.022.
|
| [35] |
范小芳,郑庆芬,周洋洋,等.Ranson评分对重症急性胰腺炎预后的预测价值[J]. 胃肠病学和肝病学杂志,2022,31(6):625-628,633. DOI:10.3969/j.issn.1006-5709.2022.06.005.
|
| [36] |
李峥艳,张凌,金涛,等. CT评分与重症急性胰腺炎合并急性肾损伤的相关性分析[J]. 四川大学学报(医学版),2011,42(5):695-698,703. DOI:10.13464/j.scuxbyxb.2011.05.016.
|
| [37] |
|
| [38] |
|
| [39] |
|
| [40] |
史武奇,张芝亚,李冰. 血肌酐与胱抑素C在慢性肾脏病诊断及评估肾功能损伤程度中的应用[J]. 解放军医药杂志,2017,29(5):89-92. DOI:10.3969/j.issn.2095-140X.2017.05.024.
|
| [41] |
吴灵萍,张萍,蒋华,等. ICU急性肾损伤患者连续肾脏替代疗法临床分析[J]. 中华危重症医学杂志(电子版),2017,10(5):322-327. DOI:10.3877/cma.j.issn.1674-6880.2017.05.006.
|
| [42] |
侯克龙,沈骁,邹磊,等. 心脏术后并发急性肾损伤的危险因素及预后分析[J]. 中国体外循环杂志,2022,20(1):25-29,43. DOI:10.13498/j.cnki.chin.j.ecc.2022.01.07.
|
| [43] |
沈云竹,熊加川,赵景宏. 小动脉透明样变与IgA肾病合并高血压患者的临床病理特征相关性分析[J]. 陆军军医大学学报,2022,44(8):805-811. DOI:10.16016/j.2097-0927.202201103.
|
| [44] |
高血压肾病诊治中国专家共识组成员.高血压肾病诊断和治疗中国专家共识(2022)[J]. 中华高血压杂志,2022,30(4):307-317. DOI:10.16439/j.issn.1673-7245.2022.04.003.
|
| [45] |
陈晨,陈园园,刘欣怡,等. ICU病人急性肾损伤危险因素的Meta分析[J]. 护理研究,2021,35(9):1588-1594. DOI:10.12102/j.issn.1009-6493.2021.09.014.
|
| [46] |
李雪芳.急诊科危重患者急性肾损伤的发生现状及危险因素分析[D]. 北京:北京协和医学院,2021.
|
| [47] |
张长春,贾晓君,张淑敏. ICU急性肾损伤的高危因素分析[J]. 临床急诊杂志,2014,15(5):262-264. DOI:10.13201/j.issn.1009-5918.2014.05.006.
|
| [48] |
毕礼明,陈英兰,陈亚峰,等. 对重症急性胰腺炎相关AKI发病机制的认识[J]. 临床肾脏病杂志,2019,19(7):539-543. DOI:10.3969/j.issn.1671-2390.2019.07.015.
|
| [1] | 秦凤银, 张绮珊, 赖锦佳, 黄奕敏, 韩郭茵, 孙兴兰, 王芬, 谭益冰. 广东省社区居民脑卒中高危筛查意向的现状及影响因素研究[J]. 中国全科医学, 2023, 26(34): 4283-4289. |
| [2] | 王喆, 董志浩, 郑好, 孔文程, 张玉宽, 张秋月, 韩晶. 针刺干预偏头痛优势方案构建研究:基于熵权TOPSIS法[J]. 中国全科医学, 2023, 26(34): 4336-4342. |
| [3] | 郝爱华, 曾韦霖, 李观海, 夏英华, 陈亮. 基于全科医生视角的家庭医生团队签约现状调查研究[J]. 中国全科医学, 2023, 26(34): 4261-4268. |
| [4] | 李殿江, 潘恩春, 孙中明, 文进博, 王苗苗, 武鸣, 沈冲. 社区2型糖尿病患者临床惰性现状及其影响因素分析[J]. 中国全科医学, 2023, 26(34): 4296-4301. |
| [5] | 王越, 陈晴, 刘鲁蓉. 中国老年人抑郁检出率及影响因素的Meta分析[J]. 中国全科医学, 2023, 26(34): 4329-4335. |
| [6] | 刘伟娜, 葛海燕, 马静, 曹琴英, 白星宇, 崔士芳, 乔彦霞. 脐血维生素A和维生素E水平与早产儿发生呼吸窘迫综合征的关系研究[J]. 中国全科医学, 2023, 26(33): 4152-4158. |
| [7] | 王丽娜, 高鹏飞, 曹帆, 葛莹, 颜维, 何岱昆. 不同性别人群非酒精性脂肪性肝病患病现况及影响因素分析[J]. 中国全科医学, 2023, 26(33): 4143-4151. |
| [8] | 李芊芊, 陈循睿, 张文颖, 袁海花, 张燕捷, 姜斌, 刘峰. 晚期肿瘤患者化疗期间对社区卫生服务需求的调查及影响因素研究[J]. 中国全科医学, 2023, 26(33): 4173-4180. |
| [9] | 梁譞, 那飞扬, 秦梦瑶, 杨辉, 郭丽, 郭琪, 任蕾, 陈德, 刘东海, 张蓉芳. 儿童支气管哮喘合并阻塞性睡眠呼吸暂停低通气综合征的临床特征及影响因素研究[J]. 中国全科医学, 2023, 26(33): 4225-4230. |
| [10] | 彰金, 丁治国, 祁烁, 李颖, 李伟强, 张媛媛, 周通. 血清甲状腺激素水平与心力衰竭患者住院期间预后的相关性研究[J]. 中国全科医学, 2023, 26(33): 4125-4129. |
| [11] | 周俞余, 高川, 崔埔安, 王亚平, 何仲. 更年期综合征患者绝经激素治疗中医患共同决策质量的影响因素研究[J]. 中国全科医学, 2023, 26(33): 4181-4186. |
| [12] | 高德康, 危少华, 马孝明, 杜鹏, 邢春根, 曹春. 肝癌大范围肝切除术后骨骼肌减少的危险因素及其与术后并发症的相关性研究[J]. 中国全科医学, 2023, 26(32): 4031-4037. |
| [13] | 王明欢, 李玉红, 俞敏, 王友刚, 俞巧稚, 杨方方, 袁德慧, 张柳. 妊娠晚期女性非稳态负荷对不良妊娠结局的影响研究[J]. 中国全科医学, 2023, 26(32): 4064-4069. |
| [14] | 袁德慧, 李玉红, 熊敏, 俞敏, 马瑞亮, 杨方方, 俞巧稚, 王明欢. 妊娠女性不同时期非稳态负荷状况及其影响因素研究[J]. 中国全科医学, 2023, 26(32): 4057-4063. |
| [15] | 李纪新, 邱林杰, 任燕, 王文茹, 李美洁, 张晋. 膳食炎症指数与超重和肥胖及腹型肥胖关系的Meta分析[J]. 中国全科医学, 2023, 26(32): 4089-4097. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||





